Cancer Has No Gender: Challenging Assumptions and Improving Quality of Care for the LGBTQ+ Community
Improve care for LGBTQ+ patients with cancer by learning about disparities, focusing on patient-centered treatment, and not making assumptions about patients and their loved ones.
Although a recent Gallup poll found the number of Americans who identify as lesbian, gay, bisexual, transgender, queer, or questioning (LGBTQ+) has doubled over the past 10 years, recent studies indicate these patients continue to face health care barriers, including disparities in oncology risk and treatment.1,2
“Unfortunately, there are still many gaps in the cancer care continuum, starting with prevention and early detection,” Diego Rodriguez, MSN, RN, OCN, senior regional nursing director at City of Hope in Duarte, California, said in an interview with Oncology Nursing News®. “LGBTQ+ patients may skip regular cancer screenings because they don’t feel welcome at certain medical facilities, especially where staff haven’t received LGBTQ+ cultural competency training. This can lead to patients being diagnosed with cancer at a later stage and limiting their treatment options.”
Diego Rodriguez, MSN, RN, OCN

As frontline caregivers, oncology nurses can improve care for LGBTQ+ patients with cancer by advocating for patient-centered treatment and creating a welcoming environment for patients and their loved ones, Rodriguez said. “By treating each patient as a unique individual with intrinsic value and dignity, oncology nurses can best serve as advocates for their LGBTQ+ patients,” Rodriguez said.
Mastering Cultural Competency
Nursing students typically do not learn about LGBTQ+ health disparities or receive cultural competency training in nursing school. One study found that 2.12 hours is the average time spent on LGBTQ+ issues in the nursing school curriculum.2
“Without the proper training and education, nurses and other health care providers can face challenges in caring for patients in the LGBTQ+ community,” Rodriguez said. “We train our nurses on inclusive practices and understand that everyone has unconscious bias that needs to be addressed.” In addition, Rodriguez said all City of Hope staff wear badge cards stating that the medical center is LGBTQ+ friendly so patients know they are welcome. Because many LGBTQ+ individuals form strong “families of choice” beyond their families of origin, Rodriguez said inclusive care should extend to each patient’s loved ones.
“We always include the patient’s companion/advocates in important conversations and ask for relationships to avoid making assumptions,” Rodriguez said. “I encourage patients to talk about the individuals they believe will best support them in their cancer journey and to have these preferences documented with health providers. Normalizing interactions with our patients, regardless of their sexual orientation or gender identity, should always be a priority.”
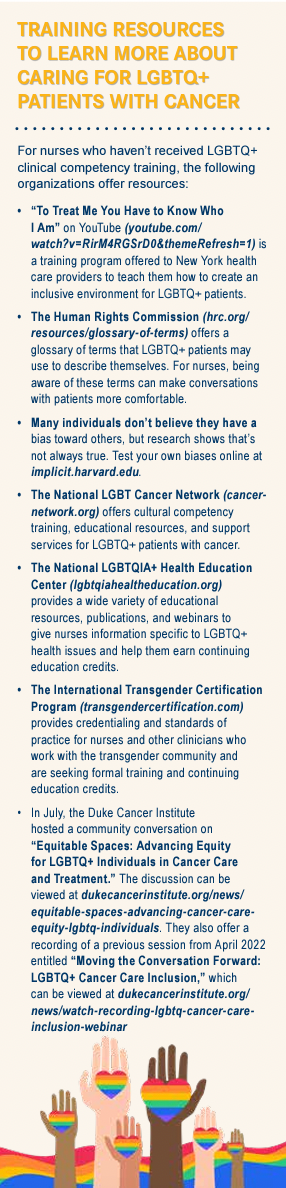
To educate nurses and other health care providers about topics such as inclusivity, biases, and preferred pronouns, the Human Rights Campaign and its partnering organizations offer more than 60 training options free to staff of Healthcare Equality Index participating facilities. The trainings include interactive courses and recorded webinars and offer continuing education credits. Oncology nurses also can seek additional training on their own (Sidebar).
Rodriguez noted that City of Hope is among 496 health care facilities presented this year with a LGBTQ+ Healthcare Equality Leader designation from the Human Rights Campaign Foundation. This is the sixth year that City of Hope has received this designation. The Healthcare Equality Index is the national LGBTQ+ benchmarking tool that evaluates health care facilities’ policies and practices related to employees, visitors, and LGBTQ+ patients.
“We achieved this distinction because of our extensive activities to sustain and nurture an inclusive and diverse workplace for both our patients and staff,” Rodriguez said. “For patients, our efforts included adding sexual orientation and gender identity questions into patient intake forms, developing new patient care policies for treating transgender and gender-nonconforming patients, training leaders in cultural awareness, updating our patient information with nondiscriminatory language, designating ‘all gender’ restrooms, and providing a care navigator for LGBTQ+ patients.”
Ensuring Health Equity
Although positive strides have been made in caring for LGBTQ+ patients, Lawrence Marsco, MSN, RN, OCN, senior director of nursing at Huntsman Cancer Institute’s Cancer Hospital at University of Utah Health, noted that barriers still exist.
Lawrence Marsco, MSN, RN, OCN

“Using inclusive language when talking to patients, taking into consideration each patient’s sexual orientation and gender identity, and using proper pronouns are very important, especially for transgender patients,” Marsco said.
For hospitals that do not collect sexual orientation and gender identity (SOGI) data for their electronic health records or intake forms, Marsco said it’s OK for nurses to ask patients how they prefer to be addressed. SOGI information typically consists of a patient’s legal name, preferred name, preferred pronouns, legal sex, and sex assigned at birth.
According to Marsco, this information is very helpful when caring for LGBTQ+ patients with cancer, especially transgender patients who may need cancer tests and treatments based on the sex they were assigned at birth rather than their current gender identity.
“Specific cancers, such as breast cancer, have no gender,” Marsco said. “Breast cancer doesn’t just affect patients who were assigned female sex at birth, it also affects men and trans women.”
One study, published in the British Medical Journal, found that trans women who received hormone therapy have an increased risk of breast cancer but may not receive information about prevention and screening.3 Last year, the American College of Radiology released transgender breast screening guidelines in an effort to improve screening in this setting.4
To make breast cancer screenings more inclusive, Marsco said it’s important that cancer centers reconsider names such as “Women’s Cancer Care” in favor of names such as “Breast Cancer Center.” He adds that it’s also important for cancer centers to incorporate SOGI forms into their admissions process and strive to create a gender-diverse cancer center. This may include providing all-gender restrooms and visible signage that reflect sexual and gender minorities, as well as relevant education materials.
When a nurse introduces themself to a patient, Marsco encourages them to say something such as, “I’m your nurse, Lawrence, and my pronouns are he/him,” followed by asking the patient, “And you are?” If a nurse does not feel comfortable using pronouns without having gone through cultural competency training, he said they can simply ask how the patient prefers to be addressed.
If a patient has a companion with them, Marsco encourages them to extend the same courtesy, rather than assuming the man accompanying the patient is his brother when it could be his husband. Rodriguez also cautioned nurses against making assumptions. As an example, he cited a study from the University of Washington School of Nursing which showed that lesbian individuals may be at higher risk of cervical cancer because they get fewer screenings than heterosexual women, due in part to health providers’ sometimes incorrect assumptions about their sexual history.5
“The LGBTQ+ community comprises diverse groups of individuals with distinct health care needs,” Rodriguez said. “Making assumptions about patients can be dangerous and lead to lapses in care.”
Identifying Barriers to Care and Improving Research
In June, a qualitative study exploring investigators’ perspectives on the health needs of LGBTQ+ patients was published in the Journal of Gay & Lesbian Social Services.6 The study identified 4 areas as the most pressing health issues facing the LGBTQ+ community. They were:
• interconnectedness of physical, mental, and social health;
• harm that discrimination causes;
• heteronormativity, or the belief that a heterosexual, cisgender identity is the only normal one; and
• health care system barriers such as insurance plans that don’t cover necessary treatments and health care providers who haven’t been trained to handle LGBTQ+ concerns.
Don S. Dizon, MD, FACP, FASCO, a professor of medicine at Brown University, director of the pelvic malignancies program and hematology/oncology clinics at Lifespan Cancer Institute, and director of medical oncology and the oncology sexual health program at Rhode Island Hospital in Providence, noted that these types of barriers, combined with a lack of SOGI data, prevent oncology caregivers from fully understanding cancer risks, adverse effects, and outcomes LGBTQ+ patients face.
Don S. Dizon, MD, FACP, FASCO

“Without collecting [these] data, it’s difficult to analyze outcomes and close the knowledge gap relating to LGBTQ+ patients and their cancer care and treatment,” Dizon told Oncology Nursing News®. “We need to ensure these patients have access to the screening programs they need and don’t delay care because they fear discrimination.”
Dizon offered a hypothetical scenario of a transgender patient assigned female at birth who now identifies as male and has breast cancer.
“Since some cancer protocols are sex/ gender specific, it can be difficult for an oncology team to know what to recommend for transgender patients,” Dizon said. “For a woman coming in on combined hormone therapy, who has been diagnosed with breast cancer, [it] would be recommended [that she stop] hormone therapy, but whether that’s the best course of action for transgender patients on gender-affirming therapy isn’t known.”
Dizon said cancer screenings can be difficult for transgender patients who may no longer identify with the organs that correspond with the gender they were assigned at birth. In addition, cancer screenings aren’t tailored to trans and gender nonconforming patients.
“We know that sexual and minority gender populations are at risk for receiving disparate care and having suboptimal experience in their cancer care,” Dizon said. He hopes that as additional cancer centers begin SOGI data collection, the information will serve to include more representation of the LGBTQ+ community in clinical trials that results in tailored cancer prevention and treatment.
“Little research has focused on LGBTQ+ health disparities,” Dizon added. “We know that anal, breast, cervical, endometrial, colorectal, prostate, and lung cancer disproportionately affect the LGBTQ+ community, but we’re still working to fully understand how cancer affects LGBTQ+ patients and the best ways to reduce these disparities.”
Resources such as the National Institutes of Health’s Sexual & Gender Minority Research Office are working to advance research for LGBTQ+ patients. In addition, the PRIDE Study (pridestudy.org), which launched in 2015, invites members of the LGBTQ+ community to participate in the first largescale, long-term national health study of LGBTQ+ individuals designed to improve the health of the LGBTQ+ community and help health care providers deliver customized, inclusive care.7 This study is being conducted by Stanford University School of Medicine in partnership with the University of California, San Francisco.
“Researchers can gain essential insights into the health and well-being of LGBTQ patients through the PRIDE study,” Rodriguez said. “Additionally, there are other studies that are ongoing at academic research centers [such as] City of Hope to help further our knowledge on how to best treat LGBTQ+ patients with cancer.”
References
1. Jones, JM. LGBT identification in U.S. ticks up to 7.1%. Gallup. February 17, 2022. Accessed November 3, 2022. https:// bit.ly/3UBswb2
2. Sherman ADF, Cimino AN, Clark KD, Smith K, Klepper M, Bower KM. LGBTQ+ health education for nurses: an innovative approach to improving nursing curricula. Nurse Educ Today. 2021;97:104698. doi:10.1016/j.nedt.2020.104698
3. de Blok CJM, Wiepjes CM, Nota NM, et al. Breast cancer risk in transgender people receiving hormone treatment: nationwide cohort study in the Netherlands. BMJ. 2019;365:l1652. Published 2019 May 14. doi:10.1136/bmj.l1652
4. Transgender breast cancer screening, American College of Radiology. 2021. Accessed November 3, 2022. https://bit.ly/3fQwBsW
5. Waterman L, Voss J. HPV, cervical cancer risks, and barriers to care for lesbian women. Nurse Pract. 2015;16;40(1):46-53. doi:10.1097/01.NPR.0000457431.20036.5c
6. Ramsey Z, Davidov DM, Abildso CG. An etic view of LGBTQ healthcare: barriers to access according to healthcare providers and researchers. J Gay and Lesbian Soc Serv. 2022;34(4):502-520. doi:10.1080/10538720.2022.2042452
7. Your story. Your health. The PRIDE Study. Accessed November 7, 2022. https://bit.ly/3Th6bP1