Knowledge of Risk Factors, Treatment Options Are Key to Managing Bladder Cancer
Significant advances have been made in diagnosing and treating bladder cancer, allowing for improved patient outcomes.
Patricia Jakel, MN, RN, AOCN

Bladder cancer is the second most common urological malignancy globally. The American Cancer Society (ACS) estimates that in 2024, there will be approximately 83,190 new cases of bladder cancer (about 63,070 in men and 20,120 in women) and an estimated 16,840 deaths from bladder cancer (about 12,290 in men and 4550 in women).1
Given that bladder cancer is common in the US, what are the causes and what can be done to help reduce this alarming number of cases? The risk factors for bladder cancer, as identified by the ACS, are listed below.2
- Smoking: Smoking is linked to about half of all bladder cancers. People who smoke are at least 3 times more likely to get bladder cancer.
- Workplace exposures: Certain industrial chemicals—such as those called aromatic amines—have been linked to bladder cancer. Industries carrying higher risks include makers of rubber, leather, textiles, and paint products, as well as printing companies. Cigarette smoking and workplace exposures can act together to cause bladder cancer. People who smoke and who also work with cancer-causing chemicals have an incredibly high risk of bladder cancer.
- Dehydration: People who drink a lot of fluids, especially water, each day tend to have lower rates of bladder cancer. This might be because they empty their bladders more often, which could keep chemicals from lingering.
- Race and ethnicity: White people are about twice as likely to develop bladder cancer as African American and Hispanic people.
- Age: The risk of bladder cancer increases with age. About 9 in 10 people with bladder cancer are older than 55 years.
- Gender: Bladder cancer rates are 4 times higher in men than in women.
- Chronic bladder irritation and infections
- Bladder birth defects
- Genetics and family history: People who have family members with bladder cancer have a higher risk of getting it themselves.
As nurses are aware, the cardinal sign of bladder cancer is visible hematuria, often accompanied by urinating more often, increased urgency, dysuria, and nighttime urination. These symptoms are not unusual in aging patients, but when accompanied by hematuria, further investigation is warranted.
After confirming hematuria, a cystoscopy with biopsy will be performed, and urine will be sent for cytology.3 If bladder cancer is diagnosed, the patient will undergo several tests: CT urogram or retrograde pyelogram, MRI, PET, and bone scan.
Types of Bladder Cancer
Bladder cancer is mainly divided into 2 categories: muscle invasive bladder cancer (MIBC) and non–muscle invasive bladder cancer (NMIBC).
MIBC
Representing approximately 25% of patients diagnosed with bladder cancer, MIBC carries a significant risk of death that has not changed in decades. The approach to these patients with MIBC should be multidisciplinary, considering the concerns of survival and quality of life.
NMIBC
NMIBC represents the majority of bladder cancer diagnoses. The survival rate is favorable for most patients with NMIBC; however, recurrence and progression to MIBC can occur and will affect long-term outcomes.
Therefore, it is critical to treat the tumor appropriately to decrease this risk.
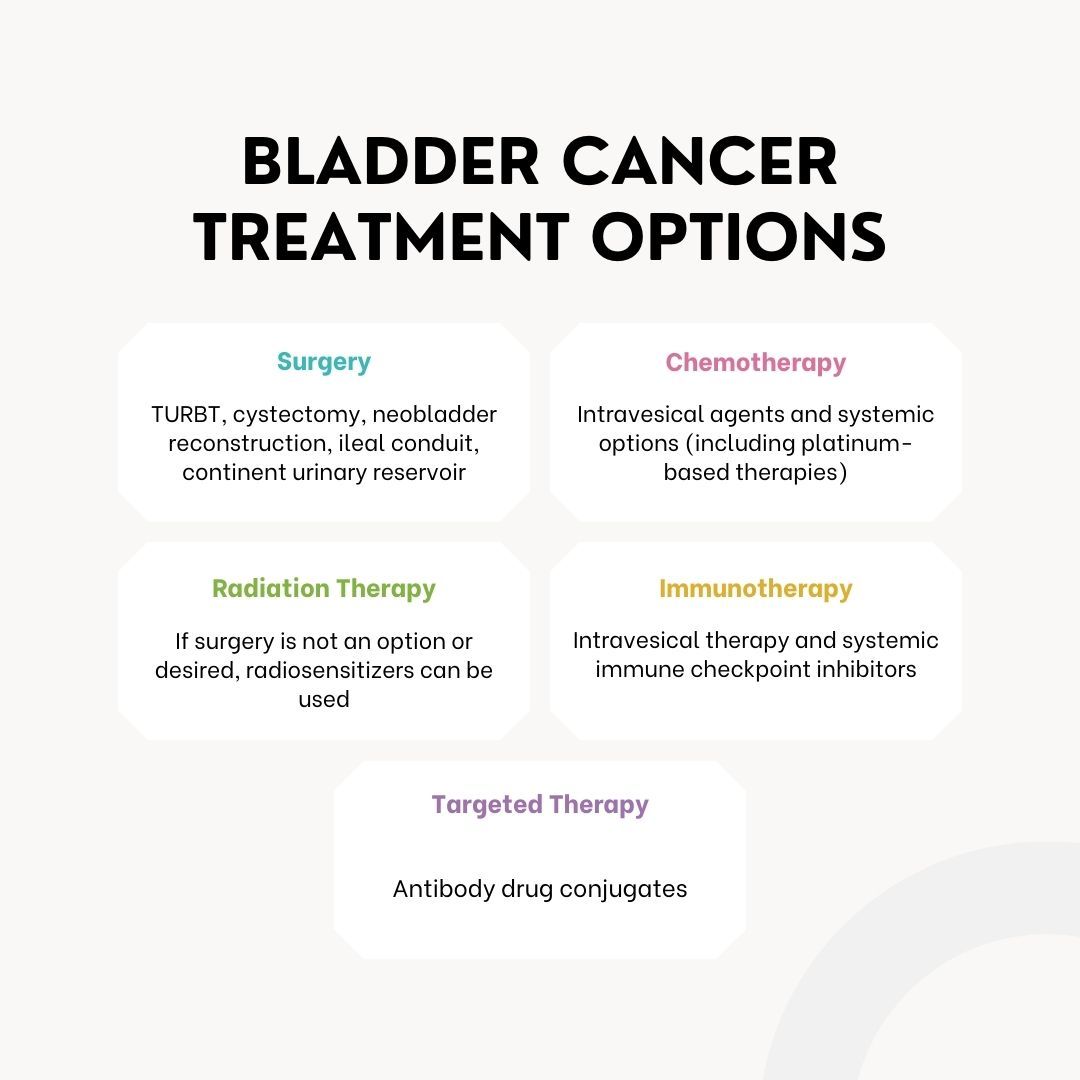
Treatment
Treatment of bladder cancer is based on pathology, stage, the status of invasion into the muscle, and various lifestyle factors. The American Urological Association (AUA) divides the guidelines into 3 categories: MIBC, NMIBC, and metastatic urothelial cancer. A multidisciplinary approach is needed to ensure adequate treatment to decrease the risk of recurrence. As the treatment of bladder cancer is complex, it is essential to utilize guidelines from major organizations such as the AUA/Society of Urologic Oncology,4 European Association of Urology, National Comprehensive Cancer Network,5 and the National Institute for Health and Care Excellence.
Conclusion
During the past 10 years, significant advances have been made in diagnosing and treating bladder cancer, allowing for improved patient outcomes. In the next 10 years, it is hoped that treatment stratification and precision medicine will enable optimal treatment with fewer toxicities, bladder-sparing surgeries, and improved quality of life.
References
- Key statistics for bladder cancer. American Cancer Society. Updated January 19, 2024. Accessed February 29, 2024. https://www.cancer.org/cancer/types/bladder-cancer/about/key-statistics.html
- Bladder cancer risk factors. American Cancer Society. Updated January 30, 2019. Accessed February 29, 2024. https://www.cancer.org/cancer/types/bladder-cancer/causes-risks-prevention/risk-factors.html
- Compérat E, Amin MB, Cathomas R, et al. Current best practice for bladder cancer: a narrative review of diagnostics and treatments. Lancet. 2022;400(10364):1712-1721. doi:10.1016/S0140-6736(22)01188-6
- Holzbeierlein J, Bixler BR, Buckley DI, et al. Diagnosis and treatment of non–muscle invasive bladder cancer: AUA/SUO guideline: 2024 amendment. J Urol. Published online January 24, 2024. doi:10.1097/JU.0000000000003846
- NCCN. Clinical Practice Guidelines in Oncology. Bladder cancer, version 1.2024. Accessed February 29, 2024. https://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf
- Immunotherapy for bladder cancer. American Cancer Society. December 19, 2023. Accessed February 29, 2024. https://www.cancer.org/cancer/types/bladder-cancer/treating/immunotherapy-for-bladder-cancer.html