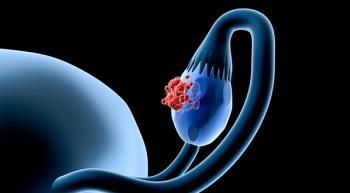
Cervical Cancer: Symptoms, Treatments, and Outlooks

Cervical cancer is often diagnosed in the later stages, though incidence of the disease is declining thanks to the HPV vaccine.
While cervical cancer rates are expected to decline thanks to the human papilloma virus (HPV) vaccine, there are still certain groups that have higher a incidence of the disease, and it is crucial for nurses to know the signs of cervical cancer, as well as the treatment modalities once someone is diagnosed.
“The key risk factor for cervical cancer is HPV,” Carolyn Grande, CRNP, AOCNP, a medical oncology nurse practitioner at the Abramson Cancer Center Hospital of the University of Pennsylvania, said in a presentation at the 4th Annual School of Oncology Nursing virtual meeting.
Risk Factors and Symptoms
“For most people, the body can clear HPV, but it can be chronic for others — especially those who have higher risk types,” Grande explained.
She noted that cervical cancer risk factors are similar to the risks of sexually transmitted diseases. This includes:
- HPV
- History of smoking
- Early age (18 years or younger) engaging in intercourse
- Number of sexual partners (5 or more) and exposure to sexually transmitted diseases
- Lower socioeconomic status
- Long-term use of oral contraceptives (5 years or longer)
While most annual cancer screenings start at an older age, the American Cancer Society recommends yearly cervical cancer screenings, which are conducted via pap test, to start at age 25, with HPV testing every 5 years.
And while the disease often starts off as asymptomatic, patients may have symptoms once the cancer grows larger. These can include: bleeding after intercourse, between periods, or after menopause; pelvic pain during intercourse; swelling in the legs; hematuria; problems moving bowels or urinating.
Cervical Cancer Treatment
Since cervical cancer usually has no early symptoms, it is often diagnosed in later stages, and can be treated with radiation, surgery, and/or chemotherapy.
“In terms of cancer treatment in advanced disease, you will have primary chemo radiation. The volume of radiation would be guided by the amount of nodal involvement. In the absence of nodal disease, pelvic radiation, external beam radiation therapy (EBRT) and concurrent platinum-containing systemic therapies and brachytherapy can be options,” Grande said.
For disease with positive para-aortic and pelvic lymph nodes, cervical cancer is often treated with extended-field EBRT, brachytherapy and concurrent platinum-containing chemotherapy.
Metastatic disease, which, unfortunately, is rarely curable, is usually treated with platinum-containing chemotherapy and palliative EBRT.
When it comes to drugs commonly used to treat cervical cancer, Grande noted the following:
First-line combination therapy
Single-agent therapy
Other agents
Cisplatin/paclitaxel/bevacizumab (Avastin)
Carboplatin/paclitaxel/bevacizumab
Cisplatin (preferred)
Pembrolizumab (Keytruda)
Cisplatin/paclitaxel
Carboplatin/paclitaxel
Albumin-bound paclitaxel
Bevacizumab
Cisplatin/topetecan
Docatexel
Larotrectinib (for NTRK gene fusion-positive tumors)
Topocecan/paclitaxel
Fluorouracil
Entrectinib (for NTRK gene-positive tumors)
Topotecan/paclitaxel/bevacizumab
Gemcitabine
Pemetrexed
As treatments evolve and more people take the HPV vaccine, cervical cancer statistics are trending toward the right direction.
“Globally, [cervical cancer] is the fourth most common cancer-related death in women. The good news, however, is that the incidence is expected to decline in women who received the HPV vaccine,” Grande said.
Reference
Grande C. Gynecologic Cancer: Essentials for Oncology Nurses. Presented at: 4th Annual School of Nursing Oncology. July 31-August 1, 2020.
Newsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.