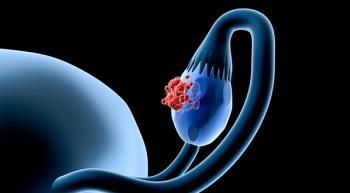
Immunotherapy in Ovarian Cancer: Don't Give Up, Yet
Robert Wenham, MD, MS, FACOG, FACS, discusses the basis for combining chemotherapy, PARP inhibitors, and VEGF inhibitors with immunotherapy in ovarian cancer and ongoing research with ADCs in the field.
Chemotherapy, PARP inhibitors, and VEGF inhibitors have all been vetted as promising combination partners for immunotherapy in ovarian cancer, according to Robert Wenham, MD, MS, FACOG, FACS, who added that only time will tell which, if any of these combinations, should make their way into clinical practice.
Although biomarker-driven approaches have fallen short of expectations, he added, the field has not given up hope that folate receptor α (FRα) could prove to be an effective target for mirvetuximab soravtansine.
“In the recurrent setting, there are some promising hints that combining checkpoint inhibition with other drugs may lead to some new [options] for patients. The challenge is going to be defining exactly which patients may get the best results from [those approaches],” said Wenham. “Biomarkers so far have been somewhat elusive. The ADCs [antibody-drug conjugates] probably hold the most promise right now, but we’re going to have to wait to see what the new results are of the mirvetuximab [soravtansine] study. Immunotherapy will [make its way into the field] but trying to figure out [how] is not going to be as simple as in some of the other cancers.”
In an interview with Oncology Nursing News' sister publication, OncLive®, during an Institutional Perspectives in Cancer webinar on ovarian cancer, Wenham, a gynecologic oncologist and chair of the Gynecologic Oncology Program at Moffitt Cancer Center, discussed the basis for combining chemotherapy, PARP inhibitors, and VEGF inhibitors with immunotherapy in ovarian cancer and ongoing research with ADCs in the field.
OncLive®: What is the rationale to combine immunotherapy with chemotherapy, PARP inhibitors, and VEGF inhibitors?
Wenham: The theoretical benefits of combining [these agents] is to make [the combination] more antigenic and to make checkpoint inhibitors work better. [Checkpoint inhibitors] work best when the immune system is stimulated and when [the checkpoint is] released from its inhibition. The idea behind combining [checkpoint inhibitors] with chemotherapy is that you are killing cells, via cytotoxic activity that’s releasing antigens and perhaps increasing the amount of antigen exposure, and at the same time chemically debulking the tumor.
In terms of PARP inhibitors, it makes sense that although they’re trying to repair DNA, you might inhibit the PARP enzyme and therefore increase the number of DNA replication errors. Then you increase number of antigens because of a poorly made product. That would increase cytotoxicity as well because you’d have more antigen exposure if you’re releasing [the] checkpoint. The combination of checkpoint inhibitors plus PARP inhibitors is an attractive [regimen].
There’s also VEGF inhibition with bevacizumab [Avastin], which has been a proven active agent in ovarian cancer. Combining that with checkpoint inhibitors is attractive, because VEGF in itself is not just an antiangiogenic molecule but may have some processes involved in the immune response, so inhibiting VEGF simultaneously with a checkpoint inhibitor [may be effective]. Also, VEGF is partly responsible for the ability for cells to migrate through vessels and for vessel stabilization.
All of these 3 different [modalities], which are active in ovarian cancer, are attractive to combine with checkpoint inhibitors. Everybody’s looking at these 3 [modalities] in combination with a checkpoint inhibitor in the frontline and recurrent settings.
What data have we seen so far that indicate such combinations are the way forward?
None of those combinations are standard of care right now. Some interesting early data have come out that may lead us in directions that we want to go. PLD [pegylated liposomal doxorubicin] plus checkpoint inhibition [has shown] about a 25% response rate and oral cyclophosphamide plus bevacizumab [Avastin] and a checkpoint inhibitor [has shown] about a 50% response rate. Weekly dose-dense paclitaxel plus a checkpoint inhibitor had about a 50% response rate. There may be some chemotherapies that may combine well with a checkpoint inhibitor, but these things need to be validated and approved before they enter widespread stream use.
Some other studies have looked at a checkpoint inhibitor plus a PARP inhibitor. The MEDIOLA study comes to mind. Besides MEDIOLA, there is the TOPACIO trial. Those studies have shown proof of principle that you can combine checkpoint inhibitors with PARP inhibitors and get responses. However, these studies have mainly been done in BRCA-mutated patients so far. We’re going have to wait to find out whether there’s a real group that benefits [outside of that subpopulation]. Part of the problem is that PARP inhibition is really good for BRCA-mutated patients, so whether a checkpoint inhibitor plus a PARP inhibitor offers an advantage over a PARP inhibitor alone [in that population] has yet to be determined.
Why are antibody-drug conjugates (ADCs) such an attractive option in ovarian cancer?
ADCs are the current state of what people are looking at in ovarian cancer. [ADCs] are attractive if you can find a selective target on a cancer cell and you can deliver a very toxic payload that you couldn’t normally give; that gives you the potential to have more efficacy [than a systemic therapy]. That’s been borne out in some of the early studies with FRα targets. There is a whole host of [studies] that are ongoing right now. There is a host of [targets] that are currently under investigation. None of these are currently standard and still need to be vetted.
The one that was furthest along was mirvetuximab [soravtansine], which [targets] FRα as well. The agent showed early activity in some of the phase 2 studies, but FORWARD I deflated some of that enthusiasm, because it didn’t meet its end point. FORWARD I evaluated platinum-resistant patients [who had received] 3 or [fewer prior] therapies. [Patients were randomized to] investigator’s choice chemotherapy, which was PLD, topotecan, or paclitaxel, or mirvetuximab [soravtansine]. However, when [the lead study author, Kathleen Moore, MD, of Stephenson Cancer Center] went back and worked with the people who are developing it, and really looked at how they did the cutoff for FRα, it appeared that changing the way that they did the analysis may have influenced the results.
When they went back to the same way that they had analyzed it [in the earlier studies], where they were looking at the intensity plus the number of high-powered [patients with FRα] vs just the intensity alone of the staining, it looked like it would have been a positive study.
However, you can’t go back and redo the rules. When you define the rules for a study, you are not allowed to go back and change it afterwards. This led to them wanting to go back and look at the exact same question again. The MARISOL study is there to answer that question but using the prior staining for levels of activity that they used in the [earlier] studies.
What other combinations are you excited about?
We give taxanes all the time, which are microbial drugs. If we’re using a taxane as an ADC or a microtubule agent, can we combine it with the same things that have shown efficacy with taxanes so far, such as bevacizumab? FORWARD II is currently looking at bevacizumab vs pembrolizumab [Keytruda] vs the combination of carboplatin and bevacizumab plus mirvetuximab [soravtansine] to see if there is additional benefit.
What can we anticipate with immunotherapy in the imminent future?
We don’t yet have immunotherapy for ovarian cancer, but we have a lot of promising leads on what may develop. The near future is going to tell us a lot. We have major phase 3 randomized trials that will be coming out in the frontline [setting] soon.
Thus far, if you look across the board, there hasn’t been one defined approach to using checkpoint inhibition for patients with ovarian cancer at this point. Some of the major up-front phase 3 studies did not meet their end point, but maybe that’s because they weren’t the right combinations. We’re going to have a lot of different views of what the right competitors and combinations are in the trials that will be reporting over the next 1 to 2 years.
This article was originally published on OncLive as, "
Newsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.