New USPSTF BRCA Recommendations Still Fall Short
While the US Preventative Services Task Force expanded their recommendations of who should be tested for BRCA mutations, there are still issues left unaddressed, according to one expert.
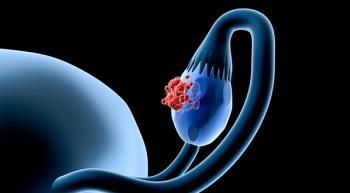
Recently, the US Preventative Services Task Force (USPSTF) expanded their recommendation of who should undergo testing for the BRCA1/BRCA2 genetic mutation, which is associated with multiple cancer types. This was a long-awaited change, according to one expert.
New Recommendations
The guidelines recommend risk assessment and genetic counseling for women with a personal or family history of breast, ovarian, tubal, or peritoneal cancers, as well as those with a family history of BRCA1/2 mutations.
“Past recommendations from the USPSTF focused on unaffected women and this is an overdue expansion of the criteria. Individuals of Ashkenazi Jewish ancestry have a 1 in 40 chance of having a BRCA1/2 mutation,” Susan Domchek, MD, Director, Basser Center for BRCA, Basser Professor of Oncology, University of Pennsylvania, said in an interview with Oncology Nursing News ®.
Addressing the Genetics-Treatment Link
However, the recommendations still leave more to be desired, according to Domchek, who co-authored an editorial in JAMA explaining that the USPSTF failed to address how genetic testing can greatly affect treatment options. In fact, the recommendations did not include newly diagnosed patients with breast and ovarian cancer or advanced-stage patients.
“Genetic testing can be very useful in individuals with newly diagnosed cancer. For example, in individuals with a new diagnosis of ovarian cancer, the presence of a BRCA1/2 mutation will lead to specific therapies. Individuals with newly diagnosed breast cancer and a BRCA1/2 mutation will discuss options such as mastectomy and oophorectomy. Men with BRCA1/2 mutations also have an increased risk of cancer and this information can be very impactful,” she said.
Further, PARP inhibitors are continuing to improve outcomes of certain patients with breast and ovarian cancer, and understanding their BRCA status is crucial in getting them the right treatment.
“All individuals with ovarian cancer should have genetic testing as they may qualify for a PARP inhibitor. PARP inhibitors are also approved for BRCA1/2-associated metastatic breast cancer. Studies have shown promising results for PARP inhibitors in BRCA1/2-associated pancreatic and prostate cancer. Thus, individuals should be tested to see if they qualify for these therapies,” Domchek explained.
More Can Be Done
Domchek went on to say that certain patients who could potentially benefit most from BRCA testing are still not being tested — and the reasons sometimes fall beyond recommendations.
“We undertest those at the highest risk and there are still significant racial and socioeconomic disparities in access and uptake of genetic testing. For example, a recent study has shown that only 30% of ovarian cancer patients have undergone testing,” she said.
Oncology nurses should identify these potential barriers and discuss genetic testing with their patients and fellow healthcare providers to ensure that all patients who need it are getting tested.
Patients can speak up and be their own advocates, too.
“Whether you have a new diagnosis of cancer, were diagnosed years ago, or have a family history, ask your healthcare provider if genetic testing makes sense for you. If you are of Ashkenazi Jewish descent, it is important that your healthcare providers know this,” Domchek said. “The value of genetic testing is its use in improving medical care. It is important that your healthcare providers help you understand your result and put it in the context of your personal and family history.”
Newsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.