- November/December 2019
- Volume 13
- Issue 9
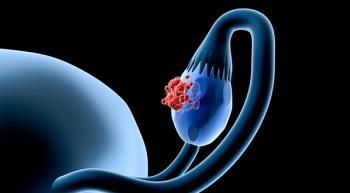
Helping Your Patients Understand and Prevent Gynecologic Cancers
Gynecologic cancers present some of the most dangerous cancer-related threats to women, here's how to help patients understand what to look out for and the realities of their treatment.
“Your final surgical pathology results confirm stage III ovarian cancer, and with your strong family history of maternal breast cancer and maternal aunt with ovarian cancer, I recommend we perform genetic testing.” As a gynecologic oncologist, this is an all too familiar conversation. Ovarian cancer is the fifth leading cause of cancer death in women, making it the deadliest of all gynecologic cancers with no screening tool. These facts are exactly why we advocate for preventive measures for ovarian cancer and the 4 other gynecologic cancers: cervical, uterine, vaginal, and vulvar.
Making sure your patient knows their family history is the first preventive step any woman can take to avoid a diagnosis of ovarian cancer. Twenty percent to 25% of all cases of ovarian cancer are due to genetic mutations, with BRCA mutations accounting for about 16% of those cases.1
Following genetic testing and in cases of a confirmed mutation, we can provide patients with preventative surgeries that remove the fallopian tubes and ovaries, dramatically reducing this risk of cancer.
Once your patient understands their genetic profile, you can help prevent the recurrence of this deadly disease by using targeted therapies proved to prolong life without disease recurrence or progression. Next up on the list of gynecologic cancers are 3 of the 5 that fall into the category of human papillomavirus (HPV)-related cancers: cervical, vulvar, and vaginal cancers.
With the development of the HPV vaccine, now available to women up to the age of 45, we can prevent these cancers and have the potential to eradicate them. Seems like a no-brainer to have your patients understand this treatment and get vaccinated. Not only does the vaccine prevent these cancers, it prevents and can help treat dysplasia, a pre-cancer that transforms into cancer of these organs if left untreated.
Finally, uterine cancer, of which endometrial cancer is a subtype, is the most common of the gynecologic cancers. A major risk factor for endometrial cancer is higher than normal estrogen stimulating the uterus, which can come from our fat tissue. Women who are overweight or obese have a much higher risk of developing this cancer. Additionally, extra estrogen exposure can come from hormone replacement therapy, which some women may start in the peri- and postmenopausal phases of life.
I focus my prevention strategies for endometrial cancer on encouraging my patients to maintain a normal body mass index with regular healthy diet and exercise; to use with caution the lowest doses for the shortest amount of time, if exploring hormone replacement therapy; and to get genetic testing if there is a strong personal or family history suggestive of Lynch syndrome.
Reference
Neff RT, Senter L, Salani R. BRCA mutation in ovarian cancer: testing, implications and treatment considerations. Ther Adv Med Oncol. 2017;9(8):519-531. doi: 10.1177/1758834017714993.
To learn more about gynecologic cancers, genetics, clinical trials, and survivorship, I encourage you to visit the Foundation for Women’s Cancer website (foundationforwomenscancer.org) and share what you learn with your family, friends, and colleagues.
Articles in this issue
about 6 years ago
Oncology Nurses Must Keep Up-to-Date to Deliver the Best Careabout 6 years ago
Medical Marijuana: Nurses's Knowledge Can Improve Patient Careabout 6 years ago
Improving Compassion Satisfaction Amid a Nursing Shortageabout 6 years ago
Vaping Presents an Old Danger to a New GenerationNewsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.