Oncology Drug Crash Course: Tucatinib and Trastuzumab for HER2+ CRC
Tucatinib was first approved by the FDA for the treatment of patients with HER2-positive advanced unresectable or metastatic breast cancer in combination with trastuzumab and capecitabine on April 17, 2020.
For a downloadable version that you can print at home, check out our oncology drug crash course page.
For Whom Is This Drug Approved?
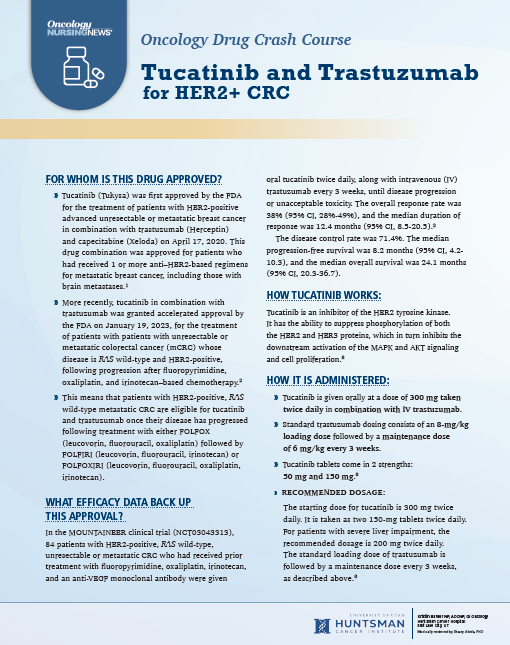
» Tucatinib (Tukysa) was first approved by the FDA for the treatment of patients with HER2-positive advanced unresectable or metastatic breast cancer in combination with trastuzumab (Herceptin)
and capecitabine (Xeloda) on April 17, 2020. This drug combination was approved for patients who had received 1 or more anti–HER2-based regimens for metastatic breast cancer, including those with brain metastases.1
» More recently, tucatinib in combination with trastuzumab was granted accelerated approval by the FDA on January 19, 2023, for the treatment of patients with patients with unresectable or metastatic colorectal cancer (mCRC) whose disease is RAS wild-type and HER2-positive, following progression after fluoropyrimidine, oxaliplatin, and irinotecan–based chemotherapy.2
» This means that patients with HER2-positive, RAS wild-type metastatic CRC are eligible for tucatinib and trastuzumab once their disease has progressed following treatment with either FOLFOX (leucovorin, fluorouracil, oxaliplatin) followed by FOLFIRI (leucovorin, fluorouracil, irinotecan) or FOLFOXIRI (leucovorin, fluorouracil, oxaliplatin, irinotecan).
What Efficacy Data Back Up This Approval?
In the MOUNTAINEER clinical trial (NCT03043313),
84 patients with HER2-positive, RAS wild-type, unresectable or metastatic CRC who had received prior treatment with fluoropyrimidine, oxaliplatin, irinotecan, and an anti-VEGF monoclonal antibody were given oral tucatinib twice daily, along with intravenous (IV) trastuzumab every 3 weeks, until disease progression or unacceptable toxicity. The overall response rate was 38% (95% CI, 28%-49%), and the median duration of response was 12.4 months (95% CI, 8.5-20.5).2 The disease control rate was 71.4%. The median progression-free survival was 8.2 months (95% CI, 4.2-10.3), and the median overall survival was 24.1 months (95% CI, 20.3-36.7).
How Tucatinib Works:
Tucatinib is an inhibitor of the HER2 tyrosine kinase.
It has the ability to suppress phosphorylation of both the HER2 and HER3 proteins, which in turn inhibits the downstream activation of the MAPK and AKT signaling and cell proliferation.3
How It Is Administered:
» Tucatinib is given orally at a dose of 300 mg taken
twice daily in combination with IV trastuzumab.
» Standard trastuzumab dosing consists of an 8-mg/kg loading dose followed by a maintenance dose
of 6 mg/kg every 3 weeks.
» Tucatinib tablets come in 2 strengths:
50 mg and 150 mg.3
» Recommended dosage:
The starting dose for tucatinib is 300 mg twice daily. It is taken as two 150-mg tablets twice daily. For patients with severe liver impairment, the recommended dosage is 200 mg twice daily.
The standard loading dose of trastuzumab is followed by a maintenance dose every 3 weeks, as described above.3
How to Manage Associated Adverse Events:
The most common adverse events (AEs) in patients receiving this combination (reported in ≥20% of patients in MOUNTAINEER) are diarrhea, rash, fatigue, nausea, abdominal pain, infusion-related reactions, and pyrexia. Common changes in laboratory values (reported in ≥20% of patients) include increases in creatinine, glucose, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, and bilirubin, as well as decreases in hemoglobin, lymphocytes, albumin, leukocytes, and sodium.2
It is important to educate your patients about the potential for diarrhea and the use of antidiarrheal agents. In our institution, we start with 2 loperamide (Imodium) at onset of diarrhea and then continue every 2 hours or with each loose bowel movement. If the patient continues to struggle with frequent bowel movements, we will escalate to diphenoxylate and atropine (Lomotil) in addition to loperamide.
Toxicities that required dose modifications in the MOUNTAINEER trial included diarrhea, hepatotoxicity, and reduced left ventricular ejection fraction.4 Fortunately, the AE-associated discontinuation rate was only 6% of patients.2
What to Inform Patients Who Are About to Start Treatment:
Of patients with metastatic CRC who were treated with tucatinib and trastuzumab (n = 86), only 4% experienced grade 3 diarrhea, and most diarrhea, 61%, was grade 1 or 2. The incidence of grade 1 or 2 fatigue was 42%; grade 3 was only 2%. Grade 1 or 2 nausea was 35%.4
Advice for Nurses Who Administer This Regimen:
There is the potential for drug-drug interactions. Pharmacists can help in reviewing a patient’s medication list. Patients should avoid strong CYP3A inducers (grapefruit juice, erythromycin) and moderate CYP2C8 inducers. Strong CYP2C8 inhibitors should also be avoided. CYP3A substrates should not be used concomitantly with tucatinib.3
Nurses should be aware that the rate of infusion-related reactions was 21%; however, these were limited to grades 1 and 2.4 Nurses should monitor for infusion-related reactions. Infusion-related reactions are typically managed by stopping the IV infusion and administering medications including antihistamines, steroids, and epinephrine as per institutional standard and resuming the infusion, if indicated, once resolved.
How to Safely Handle Tucatinib and Trastuzumab:
For handling of any chemotherapy or biotherapy medications, the recommendation from the Memorial Sloan Kettering Cancer Center is to wash your hands for 20 seconds before and after touching the medication. If a caregiver is giving patients their medications, they should use disposable gloves. No one who is pregnant or nursing should handle anticancer pills. The pills should also not be broken or crushed.5
References
1. FDA approves tucatinib for patients with HER2-positive metastatic breast cancer. FDA. News release. April 20, 2020. Accessed April 13, 2023. https://bit.ly/3ML6emm
2. FDA grants accelerated approval to tucatinib with trastuzumab for colorectal cancer. FDA. News release. January 19, 2023. Accessed February 20, 2023. https://bit.ly/3mqNcXX
3. Tukysa. Prescribing information. Seagen Inc; 2023. Accessed April 13, 2023. https://bit.ly/3L0QkmQ
4. Strickler JH, Cercek A, Siena S, et al. MOUNTAINEER: open-label, phase 2 study of tucatinib in combination with trastuzumab for HER2-positive metastatic colorectal cancer. Ann Oncol. 2022;33(suppl 4):S375-376. doi:10.1016/j.annonc.2022.04.440
5. Safe handling of chemotherapy and biotherapy at home. Memorial Sloan Kettering Cancer Center. December 12, 2022. Accessed February 20, 2023. https://bit.ly/3msoh6j