Rx Road Map: Adagrasib (Krazati)
Dawn Landolph, RN, BSN, OCN, MPA, provides an in-depth look at adagrasib for the treatment of patients with KRAS G12C-mutated, locally advanced or metastatic non-small cell lung cancer in a downloadable reference sheet.
For a downloadable version that you can print at home, check out our Rx Road Map page.
For Whom Is This Drug Approved?
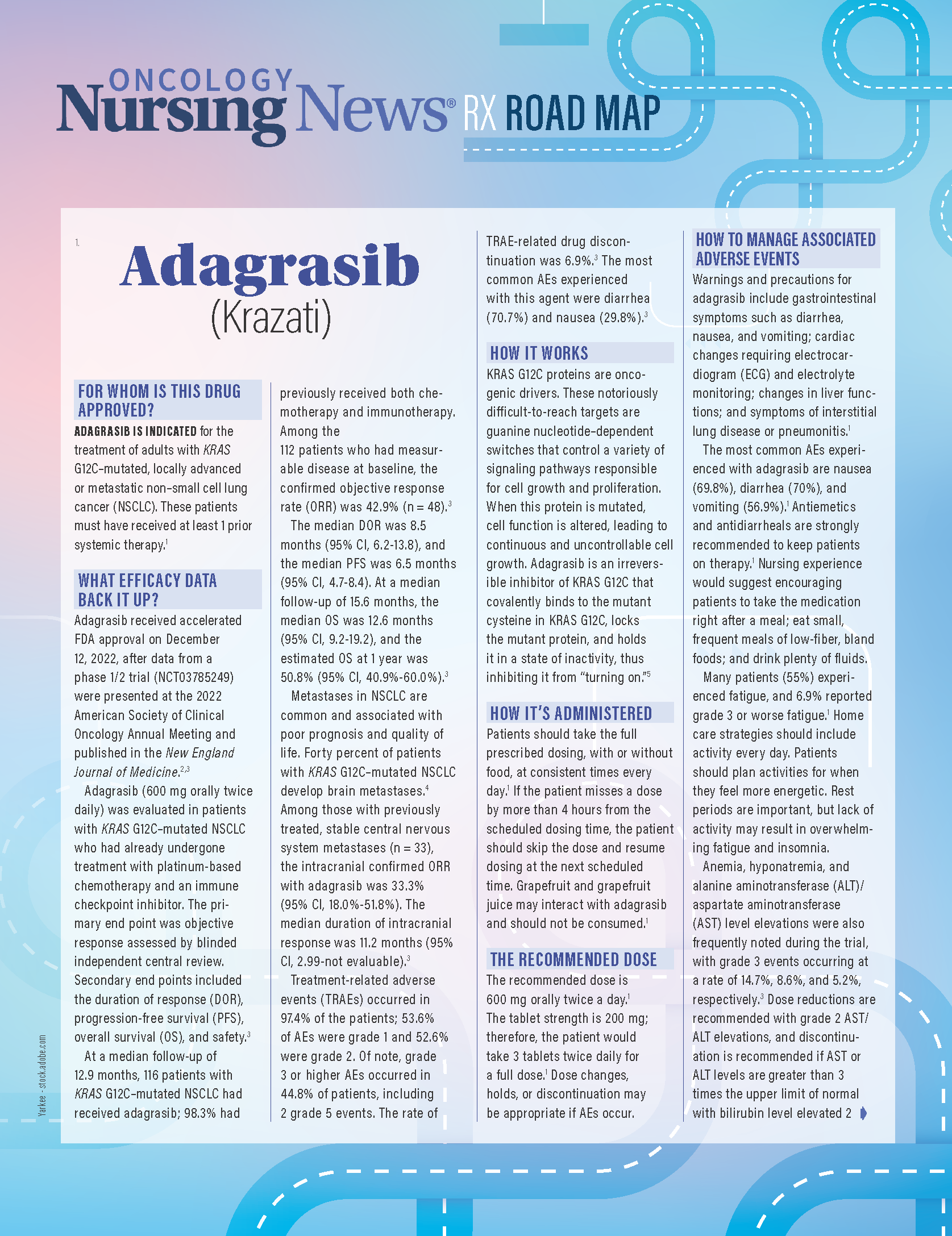
Adagrasib is indicated for the treatment of adults with KRAS G12C–mutated, locally advanced or metastatic non–small cell lung cancer (NSCLC). These patients must have received at least 1 prior systemic therapy.1
What Efficacy Data Back It Up?
Adagrasib received accelerated FDA approval on December 12, 2022, after data from a phase 1/2 trial (NCT03785249) were presented at the 2022 American Society of Clinical Oncology Annual Meeting and published in the New England Journal of Medicine.2,3
Adagrasib (600 mg orally twice daily) was evaluated in patients with KRAS G12C–mutated NSCLC who had already undergone treatment with platinum-based chemotherapy and an immune checkpoint inhibitor. The primary end point was objective response assessed by blinded independent central review. Secondary end points included the duration of response (DOR), progression-free survival (PFS), overall survival (OS), and safety.3
At a median follow-up of 12.9 months, 116 patients with KRAS G12C–mutated NSCLC had received adagrasib; 98.3% had previously received both chemotherapy and immunotherapy. Among the 112 patients who had measurable disease at baseline, the confirmed objective response rate (ORR) was 42.9% (n = 48).3
The median DOR was 8.5 months (95% CI, 6.2-13.8), and the median PFS was 6.5 months (95% CI, 4.7-8.4). At a median follow-up of 15.6 months, the median OS was 12.6 months (95% CI, 9.2-19.2), and the estimated OS at 1 year was 50.8% (95% CI, 40.9%-60.0%).3
Metastases in NSCLC are common and associated with poor prognosis and quality of life. Forty percent of patients with KRAS G12C–mutated NSCLC develop brain metastases.4 Among those with previously treated, stable central nervous system metastases (n = 33), the intracranial confirmed ORR with adagrasib was 33.3% (95% CI, 18.0%-51.8%). The median duration of intracranial response was 11.2 months (95% CI, 2.99-not evaluable).3
Treatment-related adverse events (TRAEs) occurred in 97.4% of the patients; 53.6% of AEs were grade 1 and 52.6% were grade 2. Of note, grade 3 or higher AEs occurred in 44.8% of patients, including 2 grade 5 events. The rate of TRAE-related drug discontinuation was 6.9%.3 The most common AEs experienced with this agent were diarrhea (70.7%) and nausea (29.8%).3
How It Works
KRAS G12C proteins are oncogenic drivers. These notoriously difficult-to-reach targets are guanine nucleotide–dependent switches that control a variety of signaling pathways responsible for cell growth and proliferation. When this protein is mutated, cell function is altered, leading to continuous and uncontrollable cell growth. Adagrasib is an irreversible inhibitor of KRAS G12C that covalently binds to the mutant cysteine in KRAS G12C, locks the mutant protein, and holds it in a state of inactivity, thus inhibiting it from “turning on.”5
How It's Administered
Patients should take the full prescribed dosing, with or without food, at consistent times every day.1 If the patient misses a dose by more than 4 hours from the scheduled dosing time, the patient should skip the dose and resume dosing at the next scheduled time. Grapefruit and grapefruit juice may interact with adagrasib and should not be consumed.1
The Recommended Dose
The recommended dose is 600 mg orally twice a day.1 The tablet strength is 200 mg; therefore, the patient would take 3 tablets twice daily for a full dose.1 Dose changes, holds, or discontinuation may be appropriate if AEs occur.
How to Manage Associated Adverse Events
Warnings and precautions for adagrasib include gastrointestinal symptoms such as diarrhea, nausea, and vomiting; cardiac changes requiring electrocardiogram (ECG) and electrolyte monitoring; changes in liver functions; and symptoms of interstitial lung disease or pneumonitis.1
The most common AEs experienced with adagrasib are nausea (69.8%), diarrhea (70%), and vomiting (56.9%).1 Antiemetics and antidiarrheals are strongly recommended to keep patients on therapy.1 Nursing experience would suggest encouraging patients to take the medication right after a meal; eat small, frequent meals of low-fiber, bland foods; and drink plenty of fluids.
Many patients (55%) experienced fatigue, and 6.9% reported grade 3 or worse fatigue.1 Home care strategies should include activity every day. Patients should plan activities for when they feel more energetic. Rest periods are important, but lack of activity may result in overwhelming fatigue and insomnia.
Anemia, hyponatremia, and alanine aminotransferase (ALT)/aspartate aminotransferase (AST) level elevations were also frequently noted during the trial, with grade 3 events occurring at a rate of 14.7%, 8.6%, and 5.2%, respectively.3 Dose reductions are recommended with grade 2 AST/ALT elevations, and discontinuation is recommended if AST or ALT levels are greater than 3 times the upper limit of normal with bilirubin level elevated 2 times the upper limit of normal.1 Patients should be evaluated for symptoms such as shortness of breath, chest discomfort, weakness, headaches, dizziness, jaundice, dark urine, and swelling of hands and feet.
QTc prolongation occurred in 16% of patients as reported on ECG. Common Terminology Criteria for Adverse Events grading of QTc prolongation defines grade 1 (QTc 450-480 ms), grade 2 (QTc 481-500 ms), grade 3 (QTc > 501 ms; > 60 ms change from baseline), and grade 4 (signs/symptoms of serious arrhythmia and torsade de pointes). Dose reductions or discontinuation of adagrasib should occur depending on the severity of the condition. Patients reporting palpitations or chest discomfort should be evaluated.6
Patients with worsening respiratory symptoms should be evaluated for interstitial lung disease (ILD)/pneumonitis. Adagrasib should be held in patients with suspected ILD/pneumonitis, and therapy is recommended to be discontinued if no other cause for the ILD/pneumonitis is found.1
If AEs occur, 2 dose reductions are permitted. Patients should discontinue treatment if they are unable to tolerate a 600-mg, once-daily dose.1
What to Inform Patients About
Patients should report any significant or persistent gastrointestinal symptoms, arrhythmias, heart palpitations, new or worsening cough, difficulty breathing, or fever. It is important that patients adhere to routine testing ordered by the prescriber and report any changes or new or worsening symptoms right away.1
Women should avoid breastfeeding while taking adagrasib and for at least 1 week following the last dose. Adagrasib may cause infertility and should not be used if the patient is pregnant or is planning to become pregnant.1
Grapefruit, grapefruit juice, and other CYP3A4 inhibitors may interact with adagrasib and should be avoided. Take adagrasib right after a meal or snack to reduce nausea.1 Many drugs interact with adagrasib; therefore, the patient should report all current medications and report changes in medications as soon as possible.1
Caregivers should use caution when handling adagrasib. Missed doses should be reported to the prescribing physician right away. If a dose is missed, the patient can take the dose within 4 hours of the scheduled dosing time. Patients should never take 2 doses (morning and evening doses) together.1
If patients receive the medication through mail order, health care professionals should consult the pharmacy if the agent may be exposed to temperatures lower than 59 °F or higher than 86 °F.1
Advice for Nurses Who Administer This Agent
Prior to initiating adagrasib in a patient, health care professionals should rule out pregnancy and evaluate comorbid conditions such as cardiac arrhythmias and hepatic dysfunction. It is recommended that patients with a history of congestive heart failure or bradyarrhythmia receive ECG and electrolyte evaluations prior to initiation and during concomitant use of other products known to prolong the QTc interval.1
Monitoring of liver function tests (AST, ALT, alkaline phosphatase, and total bilirubin) at least monthly for the first 3 months is recommended. Patients with transaminase level elevations should be monitored more frequently. Median time to elevation is approximately 3 weeks. Baseline and regular monitoring of the completed blood count should be performed because anemia, thrombocytopenia, leukopenia, or neutropenia may have occurred.1
Baseline gastrointestinal symptoms and stooling patterns should be evaluated. Patients’ baseline respiratory condition should be noted and regularly monitored for worsening breathing issues; ILD has been noted to present on average at 12 weeks following initiation of treatment.1
Adagrasib has many drug interactions; therefore, a detailed medication reconciliation should be performed prior to starting therapy.1
How to Safely Handle This Agent
Adagrasib should be stored in its original bottle. The tablets should be stored at room temperature. Patients should never break, split, crush, or chew the tablets.1 They should report any broken or damaged medication to their pharmacy right away. Caregivers should wear gloves if administering the medication to the patient.
References
- Krazati. Prescribing information. Mirati Therapeutics Inc; 2022. Accessed November 21, 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/216340s000lbl.pdf
- Zhang J, Johnson M, Barve M, et al. Practical guidance for the management of adverse events in patients with KRASG12C-mutated non-small cell lung cancer receiving adagrasib. Oncologist. 2023;28(4):287-296. doi:10.1093/oncolo/oyad051
- Jänne PA, Riely GJ, Gadgeel SM, et al. Adagrasib in non-small cell lung cancer harboring a KRAS G12C mutation. N Engl J Med. 2022;387(2):120-131. doi:10.1056/NEJMoa2204619
- Lamberti G, Aizer, A, Ricciuti B, et al. Incidence of brain metastases and preliminary evidence of intracranial activity with sotorasib in patients with KRASG12c-mutant non-small-cell lung cancer. JCO Precis Oncol. 2023;7:e2200621. doi:10.1200/PO.22.00621
- Addeo A, Banna GL, Friedlaender A. KRAS G12C mutations in NSCLC: from target to resistance. Cancers (Basel). 2021;13(11):2541. doi:10.3390/cancers13112541
- CTEP Cancer Therapy Evaluation Program. National Cancer Institute. Accessed April 19, 2021. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm#ctc_50