Symptom Assessments, Guidelines Inform Nurses Whether They Are ‘Moving in the Right Direction’ in MPN Treatment
Tetyana Furmanets, CRNP, MSN, discusses the tools she uses to help patients navigate myeloproliferative neoplasm symptom management.
Tetyana Furmanets, CRNP, MSN

Although patients with myeloproliferative neoplasms (MPN) often experience many symptoms either related to the disease or from treatment itself, nurses can help patients navigate symptom management and help seek relief, one expert said.
Oncology Nursing News® spoke with Tetyana Furmanets, CRNP, MSN, an oncology nurse practitioner at Penn Medicine Abramson Cancer Center in Philadelphia, to learn more about how nurses can advise patients with MPN on symptom relief and tools available for nurses to gauge treatment responses.
Oncology Nursing News: What are some of the symptoms associated with MPN and what are some ways nurses can help patients manage them?
Furmanets: MPN comes with a lot of symptoms, the most prominent one being probably fatigue. A lot of patients report debilitating, generalized fatigue. That is probably one of the hardest ones to manage as well because there's no specific targeted agent for that. I recommend [that] our patients continue to exercise as much as possible while listening to their body, going on daily walks while taking time to rest at home. Certain medications that patients are taking for MPN might help with the symptoms of fatigue.
Some of the other symptoms that we see with myeloproliferative neoplasms are itching. That’s one of the big ones. Specifically, patients report severe itching after they take a shower. Our recommendation is either lowering the temperature of the water before taking a shower or using topicals. There is one lotion—which is over the counter—that we use a lot, Sarna cream, which is very helpful for our patients. We recommend applying that after taking a shower while their skin is still wet.
There are some side effects of the myeloproliferative neoplasms that are very tricky to deal with. Some of them may be fevers, which you can take Tylenol, but there comes a point of the disease process where Tylenol is just not helping with it. So promote fluids, hydration. Sometimes that can be very helpful with symptoms of fevers as well as bone pain, which we see a lot with this patient population as well.
Some of the more vague symptoms that we see is difficulty with concentration, which is a little hard to get out of the patients to talk more about, but when you ask them about it, they’re like, ‘I definitely started noticing I'm having more issues with that.’ This one is a little harder to treat. But I feel like going for those walks and trying to like breaks, take rest and listen to your body and don't push it too hard, have been definitely helpful.
The other big one we see with myeloproliferative neoplasms is getting full after a few bites of food. A lot of patients are not able to finish full meals because of their spleen size. They have some discomfort associated with their spleen. That comes hand in hand along with fatigue and is probably one of the biggest symptoms we see in this patient population. Again, some of the treatments help with reducing the spleen size. When patients do experience that, they're so grateful and they feel amazing. They're like, ‘I could finally finish a full plate and I'm able to sleep on that side.’ So that's very encouraging.
Unfortunately, sometimes patients don't respond that well to treatment, so they’ll experience some of that left-sided abdominal pain. We work with nutritionists a lot for those patients; we encourage them to [try] some small, frequent meals that are high-protein, high-calorie content, so that even though they're not getting a lot of food in at one time, they are still getting their adequate nutrition and their caloric amount during the day.
We work a lot with our palliative care team to help with the pain management aspects when we get to severe cases of myelofibrosis. Pain medication might help with that, as well [as] avoiding sleeping on that side, avoiding certain types of activity or exercise to avoid more trauma to the spleen.
Are there tools that nurses can use to educate their patients about the side effects?
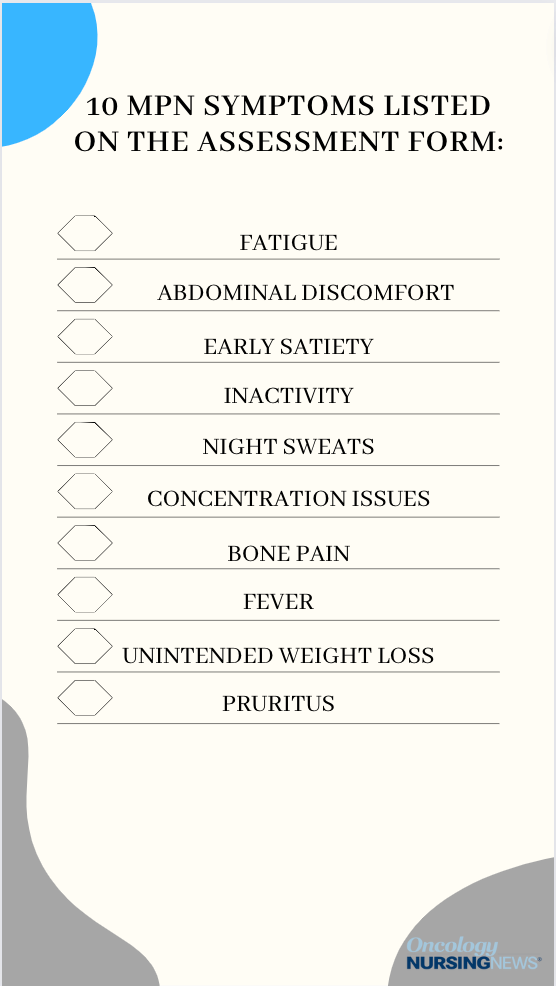
I utilize NCCN guidelines a lot during the treatment phase. We use an MPN treatment symptom assessment during our visits. It's a questionnaire; patients score [their symptoms] on a scale from zero to 10, zero being no symptoms at all and 10 being the worst imaginable. It lists all of the most common symptoms, fatigue, pain, itching, abdominal pain. It is very helpful as far as determining where the patients are on the scale of the severity.
It might be beneficial if the nurses utilize it and give it to the provider, something to compare it to because a lot of times when you ask the patients, how are you feeling and they're telling you they feel fine. And when you give them the questionnaire it's like everything's like nine or 10 out of 10, so you have to dig a little deeper with those questions.
It is a very tricky disease to manage because everybody's so different as far as that goes. But we have been utilizing that symptom assessment form a lot and have been helpful to determine if we're moving in the right direction or making any progress, if we are addressing those symptoms at all.
What's the most important thing for nurses to keep in mind when caring for patients with MPN who are experiencing symptoms?
Unfortunately, a lot of treatments don't work overnight. It takes weeks to a month to fully kick in. It can be very frustrating for our patients. We have a lot of patients who are coming in and reporting that they just started this medication, they're still not feeling too great, and they get a little discouraged. Reinforce that it might take some time for the medication to kick in.
Transcription has been edited for clarity and conciseness.
Do you know an oncology nurse who goes above and beyond to identify and manage symptoms of patients with MPNs? Submit your nomination for the 2024 Extraordinary Healer® Award for Oncology Nursing.
Nursing Perspectives on Managing Toxicities With ADCs in Metastatic Gastric and Breast Cancers
September 1st 2022In this episode of "The Vitals," Sarah Donahue, MPH, NP, AOCNP; Jamie Carroll, APRN, CNP, MSN; Theresa Wicklin Gillespie, PhD, MA, RN, FAAN; and Elizabeth Prechtel-Dunphy, DNP, RN, ANP-BC, AOCN, exchange clinical pearls for treating patients receiving antibody-drug conjugates.



