
Managing Patients With Low-Risk MDS on Luspatercept
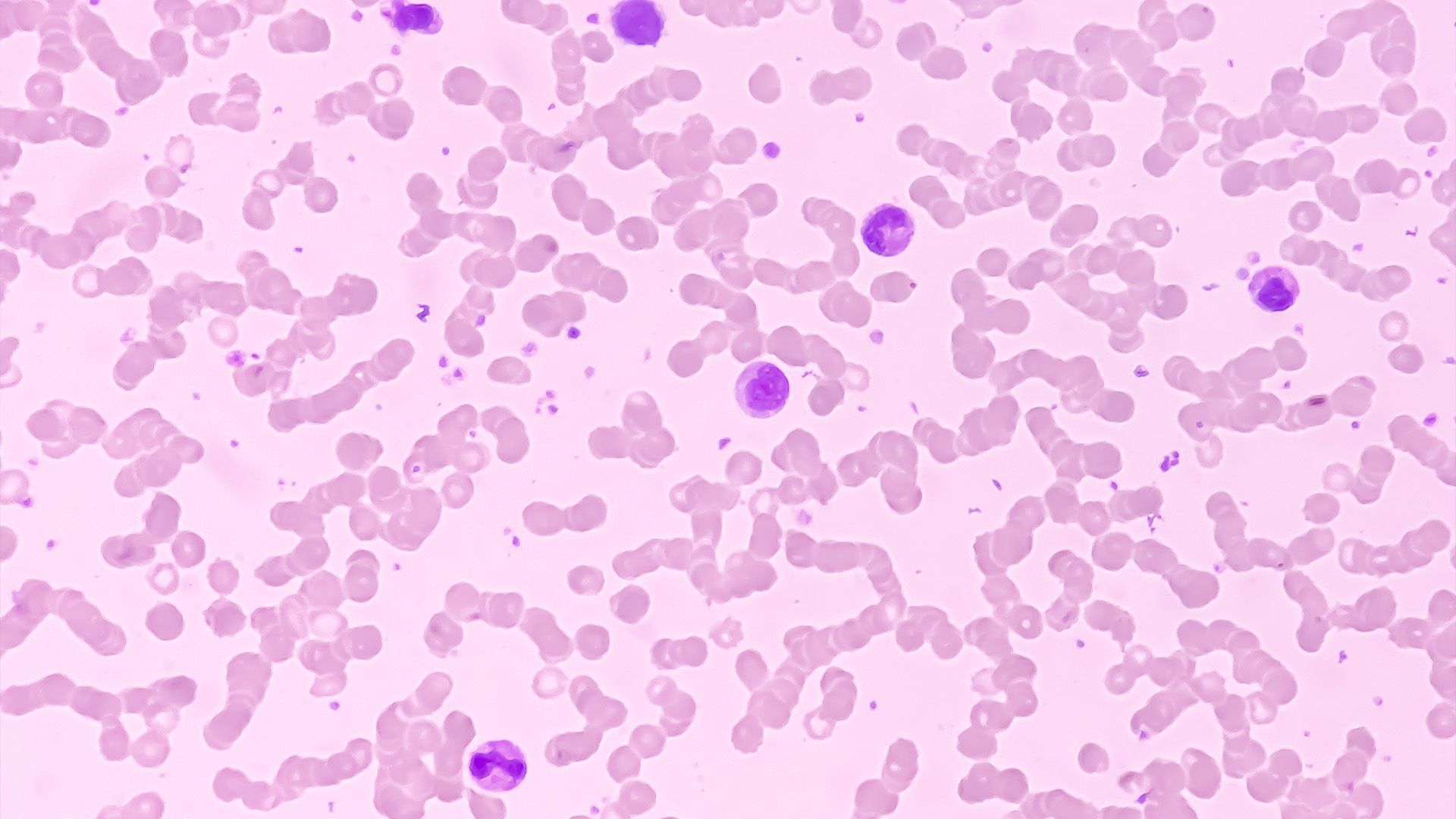
Elizabeth Hubert, APRN, explains how to treat patients receiving luspatercept for low-risk myelodysplastic syndromes.
Treating patients with low-risk myelodysplastic syndromes (MDS) may require titration or other considerations in disease management to avoid the onset of adverse effects (AEs), as Elizabeth Hubert, APRN, explained in an interview with Oncology Nursing News following a Case-Based Roundtable.
Luspatercept-aamt (Reblozyl) is among the National Comprehensive Cancer Network (NCCN) guideline recommendations for low-risk MDS. However, luspatercept can cause asthenia, a debilitating version of fatigue that makes it difficult for patients to move. Along with asthenia, luspatercept can be associated with diarrhea and muscle aches and pains.
For patients experiencing issues with luspatercept, Hubert, an MDS nurse practitioner at The University of Texas MD Anderson Cancer Center in Houston, explained that titration and steroid boosts can help patients overcome AEs and remain on treatment.
What is the role of advanced practice providers in managing low-risk MDS?
All of us work in hematology oncology, and one of the things we could agree on is that, across the board, we get a lot more face time with the patients, so we have a lot more opportunity to hear their side of the story and hear about the [adverse] effects of whatever therapy they’re on, and then go over the considerations of the titration. The consensus is that we are responsible for the titration in coordination with the physician and the pharmacist. It’s not a unilateral decision for anyone, but they are also mostly in charge of managing the adverse effects from the therapies.
When are treatments for low-risk MDS titrated?
There is a role for the titration of [erythropoiesis-stimulating agents (ESAs).] However, mostly what we’re going to be titrating is luspatercept, and it has a very straightforward way to titrate it from 1 to 1.3 to 1.75 mg/kg. You can also dose reduce and titrate it down if the patient’s [experiencing] some adverse effects, such as asthenia, diarrhea, muscle pain, anything like that. We also talked about when to discontinue one therapy and switch to another one. We wanted to make sure we optimized [treatment] by doing the full titration before discontinuing [it]. The other agent we could titrate would be imetelstat (Rytelo). We would titrate that agent down as well. That decision would be [made] more [by] the pharmacist and the physician.
Does luspatercept come with any adverse effects?
The biggest AES with luspatercept that we noticed in personal experience and in the studies was fatigue. The asthenia is a huge one. Asthenia, for those who don’t know, is an awful, horrible, overwhelming fatigue, where you don’t want to move your arms and legs, and it’s very concerning to the patients, because they feel so terrible. The big [AEs] are fatigue, diarrhea, and muscle aches and pains.
How are the AEs of luspatercept best managed?
We talked about sometimes giving a small steroid boost. When you’re giving the dose, you can also reduce the dose. Instead of starting them at 1 mg/kg, start them at 0.7, 0.5, or 0.8 mg/kg, and help them through. Those AEs should reduce as they get further along in the therapy. They’re usually the worst at the very initiation of the therapy, so we must help them through that period.
What special considerations should be taken in managing cytopenias in low-risk MDS?
One of the things we’re going to take into consideration is, do they have just the single cytopenia, which is anemia? Or do they have multilineage, where they have neutropenia, thrombocytopenia, or [issues along] all 3 lines? [In that case,] we would probably go more toward a hypomethylating agent, but you could still add in or use luspatercept or ESA in addition to it.
When should care teams move from ESAs to luspatercept?
In accordance with the NCCN guidelines…many people are using ESAs for an undetermined amount of time before considering it a failure. They didn’t only have 12 weeks or 6 weeks. How many times do we give it before we call it a failure? When does luspatercept come into play? I am of the mindset that luspatercept can be used as an earlier intervention than it is now.
This transcript has been edited for clarity and conciseness.
Newsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.































































































