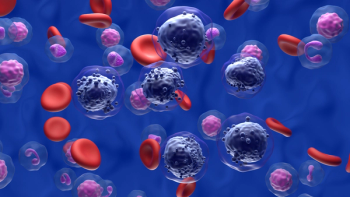
Hematology
Latest News

Lower Rates of ICANS, CRS 2 Weeks After CAR T May Support Shorter Monitoring Period for DLBCL
Latest Videos

More News

The FDA granted the investigational menin-MLL inhibitor DSP-5336 fast track designation for KMT2A-rearranged/NPM1-mutant acute myeloid leukemia.

Ciltacabtagene autoleucel demonstrated a statistically significant improvement in overall survival for patients with relapsed/refractory multiple myeloma refractory to lenalidomide.

Three-year findings from the TRANSFORM trial provide further evidence that liso-cel should be considered as the new standard of care along with other CAR T-cell therapies for patients with primary refractory or relapsed LBCL, an expert said.

The updated risk evaluation and mitigation strategies for autologous CAR T-cell therapy removed requirements for training and educational materials about the risk for certain toxicities.

Improving progression-free survival and confirming results with MRD testing were treatment qualities that patients with CLL reported were more important than other factors.

Adding ibrutinib to chemoimmunotherapy induction with autologous stem-cell transplantation improves failure-free survival rates in younger patients with mantle cell lymphoma.

Patients with previously untreated chronic lymphocytic leukemia treated with venetoclax plus obinutuzumab either with or without ibrutinib experienced significant PFS improvements.

Throughout June, the FDA approved drugs for the treatment of diseases including myelodysplastic syndrome, thyroid cancer, endometrial cancer, colorectal cancer, and follicular lymphoma.

Treatment with linvoseltamab provided durable efficacy for patients with relapsed/refractory multiple myeloma.

Compared with epoetin alfa, treatment with luspatercept improved erythroid response rates and the duration of transfusion independence for lower-risk myelodysplastic syndromes.

An accelerated approval has been granted by the FDA to epcoritamab-bysp (Epkinly) for adult patients with relapsed or refractory follicular lymphoma after 2 or more lines of systemic therapy.

The administration of CAR T-cell therapy in an outpatient setting was deemed feasible and safe for patients with relapsed/refractory non-Hodgkin lymphoma.
Oral azacitidine had a similar safety profile across the 200-mg and 300-mg groups in lower- to intermediate-risk MDS.

The FDA granted an approval to imetelstat for certain patients with low- to intermediate-1-risk MDS who have transfusion-dependent anemia.

Oncology nurses can aid in the identification and management of oral adverse effects from cancer therapies.
Triplet therapies containing belantamab mafodotin, pomalidomide, and dexamethasone may address an unmet need for relapsed/refractory multiple myeloma.

Updated data from the MANIFEST-2 study support a paradigm shift in the treatment of JAK inhibitor–naive patients with myelofibrosis.

A brentuximab vedotin-containing regimen led to “unprecedented” progression-free survival improvements in patients with advanced classical Hodgkin lymphoma.

Asciminib led to a superior 48-week major molecular response rate compared with investigator-selected tyrosine kinase inhibitors for Ph-positive chronic phase chronic myeloid leukemia.

This marks the only CAR T-cell therapy approved by the FDA for 4 subtypes of non-Hodgkin lymphoma.

Oncology nurses can educate patients about the availability of pre-exposure prophylaxis for preventing COVID-19.

Uproleselan plus chemotherapy missed the overall survival end point in the phase 3 trial assessing the combination in patients with relapsed/refractory acute myeloid leukemia.

Second-line venetoclax may lead to monthly cost savings vs second-line BTK inhibitor for patients with chronic lymphocytic leukemia or small lymphocytic lymphoma.

Lisocabtagene maraleucel was approved by the FDA to treat adults with relapsed/refractory follicular lymphoma who were treated with 2 or more prior lines of systemic therapy.

Recent data from a phase 3b trial support venetoclax as a CLL treatment option for those with or without B-cell receptor–associated kinase inhibitor treatment.