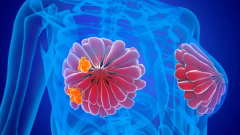
CDK4/6 Inhibition Customizes Frontline HR+, HER2- mBC Treatment
According to Kimberly Podsada, BSN, RN, MSN, NP-C, CNS, the availability of 3 CDK4/6 inhibitors in first-line mBC therapy gives patients more choices.
Episodes in this series

Because of the selection of CDK4/6 inhibitors now available in the first-line setting for patients with hormone receptor (HR)-positive, HER2-negative metastatic breast cancer, providers now have the option to tailor treatment to patients’ preferences and history, according to Kimberly Podsada, BSN, RN, MSN, NP-C, CNS.
In an interview with Oncology Nursing News following a Case-Based Roundtable discussion with fellow oncology advanced practice providers (APPs), Podsada explained that a patient’s prior experiences such as suboptimal liver function, nausea during pregnancy, or rheumatoid arthritis could impact a provider’s choice of
Podsada, a nurse practitioner at the University of California San Diego, emphasized that these options allow providers to make a more personalized and informed care decision with patients.
Transcript
We have the luxury now of having a
There are our
One of the things I like to assess about my patients are the baseline issues that they’re already bringing into clinic: “I already have a sensitive gut.” “Oh, I had really bad nausea with pregnancy.” “I’m already on an immunosuppressant for my rheumatoid arthritis.” All of these things I’d be looking at and making a decision.
If someone’s coming off of chemotherapy, let’s say, and they still have [gastrointestinal] issues and they were never able to get on top of their diarrhea, am I going to prescribe
It’s a very detailed conversation with the individual and looking at the whole person honestly and thinking about that, not just having your personal preference of, “This is the drug I always want to prescribe,” but looking at the patient and going, “How is this medication going to impact my patient’s quality of life and ability to get the best care I want to give her or him?”
This transcript has been edited for clarity and conciseness.
Newsletter
Knowledge is power. Don’t miss the most recent breakthroughs in cancer care.