
New findings suggest that neoadjuvant therapy with antibody-drug conjugates may be effective for patients with early-stage breast cancer.

New findings suggest that neoadjuvant therapy with antibody-drug conjugates may be effective for patients with early-stage breast cancer.
A triplet regimen of tucatinib, trastuzumab, and capecitabine helped patients with HER2-positive metastatic breast cancer and brain metastases live longer with reduced disease progression compared with trastuzumab and capecitabine alone.

PI3K-pathway mutations may predict an increased risk of secondary uterine cancer in patients receiving tamoxifen to treat primary breast cancer.

Updates from the ongoing INSEMA trial suggest that patients with early-stage breast cancer maintain superior quality of life by forgoing sentinel lymph node biopsy and axillary lymph node dissection.

Findings from a breast cancer analysis demonstrated that pathologic complete response and event-free survival rates were not significantly affected by patient’s race.
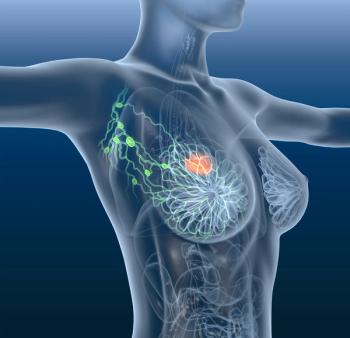
The introduction of adjuvant approaches reduced the risk of disease recurrence in HER2-positive, early-stage breast cancer.

Treatment modifications were inconsistent among White and Black patients with breast cancer. However, the use of a multiscale biophysical modeling platform may be useful in informing treatment modification decisions.

Aromatase inhibitors were revealed to be more effective than tamoxifen in reducing the rate of recurrence in ER+ breast cancer among premenopausal women receiving ovarian suppression.
The 24-month lymphedema rate was 39.4% among Black women, making it the highest incidence rate in any category.

Patients who received matched targeted therapy specific to their genomic alteration, as identified through multigene sequencing, experienced significantly improved progression-free survival.

Nearly 1 year following the first checkpoint inhibitor approval in advanced triple-negative breast cancer, additional immunotherapeutic agents are poised to enter the field, according to Rita Nanda, MD.

Results of a new study show that adding ribociclib (Kisqali) to standard endocrine therapy with temporary ovarian suppression significantly improved progression-free survival (PFS) when used as a first-line treatment for