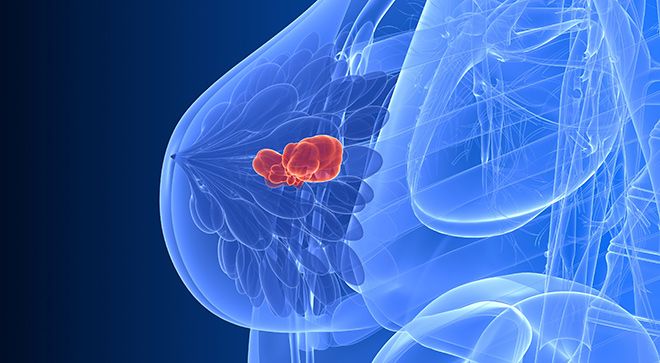
Based on data from the phase III MONARCH 3 trial, the FDA has approved abemaciclib (Verzenio) for use in combination with an aromatase inhibitor for the frontline treatment of postmenopausal women with hormone receptor (HR)-positive, HER2-negative advanced or metastatic breast cancer.