
There are still no simple answers to the question of screening for prostate cancer.

There are still no simple answers to the question of screening for prostate cancer.

Broad-based genomic sequencing, while useful in identifying tumor mutations in patients with non-small cell lung cancer (NSCLC), may not improve survival outcomes when compared to routine genomic testing.

Next-generation sequencing (NGS) in metastatic non–small cell lung cancer (NSCLC) can save Center for Medicare and Medicaid Services (CMS) payers $1.4 million to $2.1 million.

Mail-in DNA tests may not provide enough information to people looking for answers about their genetic predisposition to cancer.

A shortage of genetic counselors inspired researchers to find a way to streamline testing to prevent delays in treatment for patients with ovarian cancer who require BRCA testing.

Genetic testing for cancer may result in unforeseen revelations.

Direct-to-consumer genetic testing enables individuals to pursue testing independently and without interference from a healthcare professional. But is there a downside?

Based on results from the phase III OlympiAD trial, the FDA approved olaparib (Lynparza), a PARP inhibitor, for the treatment of patients with germline BRCA-positive, HER2-negative metastatic breast cancer who have previously received chemotherapy. HR-positive patients must also have had prior endocrine therapy.
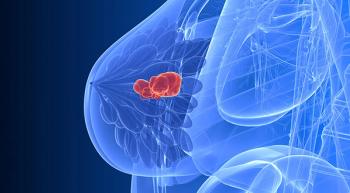
The combination of olaparib (Lynparza) and durvalumab (Imfinzi) for pretreated patients with germline BRCA-mutated (gBRCAm), HER2-negative metastatic breast cancer shows great promise for future treatment.

Megan Hoffman, MSN, RN, CMSRN, AOCNS, discusses the importance of nurse's understanding genomics so their patients can get the full benefit.

A recent study has shown that the cancer risks for women with BRCA1 and BRCA2 mutations depend on the extent of the woman’s family history of cancer and the position of the specific fault within the gene.

Megan Hoffman, MSN, RN, CMSRN, AOCNS, discusses the importance of having a nurse's perspective when discussing genomics and precision medicine.

Krista Qualmann discusses hereditary cancer syndromes.

Krista Qualmann explains what a meeting with a genetic counselor will look like for a patient.

A recent study found that young women with breast cancer who are BRCA-positive have similar, or better, outcomes than those who do not, and that preventative bilateral mastectomy in this population does not improve the risk for recurrence or death.

Krista Qualmann discusses the nurse's role once a patient has gone for genetic testing.

Expert Kristin Zorn, MD discusses the importance that genetics plays in oncology, and the why genetic counseling and testing are vital.

Dr. Erin Hofstatter gives some "red flags" that indicate a patient or family member should consider genetic counseling and testing.

Genetic testing can be used to stratify the risk of a patient experiencing complications during cancer, such as venous thromboembolism (VTE).

In a recent phase III study, the PARP-inhibitor olaparib was shown to improve progression-free survival for patients with BRCA-positive ovarian cancer.

The Society for Gynecologic Oncology (SGO) released a toolkit of case studies and resources on genetic testing for healthcare providers, patients, and their families.

Cathy Belt, RN, MSN, AOCN, Abramson Cancer Center of the University of Pennsylvania, discusses possible steps individuals can take upon finding out they have an inherited cancer syndrome, such as mutations in the BRCA1 or BRCA2 genes.

With approximately 5% to 10% of cancers attributable to a hereditary cancer predisposition syndrome, identifying those patients with cancer who are at risk has significant benefit both to patients and their relatives.

Ignacio I. Wistuba, MD, chair of the department of Translational Molecular Pathologies at MD Anderson Cancer Center, discusses the role nurses play in the field of molecular testing.

What do patients think about being tested for many genes that may impact their hereditary risk for breast or ovarian cancer, beyond the well-known BRCA mutations?

A study involving women with a BRCA mutation who had risk-reducing surgery to lower their risk of breast and/or ovarian cancer found that many of these individuals have surgical procedures such as oophorectomy or mastectomy without a full understanding of how they will affect their sexuality and other aspects of their lives.

Mark E. Robson, MD, Clinical Director of the Clinical Genetics Services at Memorial Sloan Kettering Cancer Center, discusses when it is appropriate to go for genetic testing to determine cancer risk.

Debu Tripathy, MD, chair of the Department of Breast Medical Oncology at University of Texas MD Anderson Cancer Center, discusses the potential for using breast cancer tumor DNA to make treatment decisions.

National guidelines recommend that women with a personal history of ovarian cancer be tested for the BRCA mutation. Approximately 1.3% of women will develop ovarian cancer, according to the National Cancer Institute, but that risk increases to an estimated 39% in women with the BRCA1 mutation and 11% to 17% in women who inherit the BRCA2 mutation.

Young black women with breast cancer are much less likely to have BRCA testing or, if they carry a BRCA mutation, to undergo risk-reducing prophylactic mastectomy or salpingo-oophorectomy.