
An hourly rounding column helped make integrated data points more visible and improve nurse responsiveness on an inpatient floor.

An hourly rounding column helped make integrated data points more visible and improve nurse responsiveness on an inpatient floor.
Stephanie Jackson, DNP, MSN, RN, AOCNS, BMTCN, discusses how collaboration between an oncology unit and discharge lounge can improve discharge times for patients who have undergone stem cell transplantation.

A medication extension set may be the preferred method for subcutaneous hyaluronidase injections compared with a traditional needle.

Michelle Mollica, PhD, MPH, RN, OCN, senior advisor in the NCI Office of Cancer Survivorship, discusses different long-term care considerations for nurses caring for patients with cancer.
Brianna Lutz, MSN, RN, OCN, discusses a red-and-green dot hourly column that shows which patients with cancer have been attended to in the past hour.
Patricia Jakel, RN, MN, AOCN, discusses burnout and compassion fatigue in acute oncology care.

Conversations surrounding fertility preservation may differ between young men and women with cancer, according to Donna Herrera Bell, MSN, APRN, FNP-C.
Kate Sandstrom, MSN, APRN-BC, AOCN, discusses the importance of including the radiation oncology team in a patient’s long-term care plan.
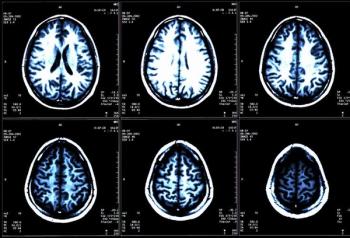
Unrelieved stress may contribute to cancer-related cognitive impairment and anxiety in patients undergoing chemotherapy.

In the age of cyberattacks, establishing and practicing a downtime procedure is crucial to safeguard patient care, according to Kelli-Ann Mancini, MSN, RN, OCN.

A nurse-led intervention demonstrated initial success in connecting patients to scalp cooling therapy and reducing the impact of alopecia.

Older men who have received androgen-deprivation therapy are an increased risk of heart issues, however, the root of the risk is still not well understood.

Cognitive therapies were found to be effective for helping cancer survivors with insomnia, but more research is needed for patients actively receiving treatment.

Oncology nurses may be able decrease peripheral access wait times for patients, however, a change in culture may be necessary to see full results.
Jessica MacIntyre, ARNP, NP-C, AOCNP, discusses empowering oncology nurse navigators to refer patients undergoing chemotherapy or radiation therapy to nutrition services.
Niraparib improved or maintained health-related quality of life, pain intensity, and pain interference in patients with advanced or metastatic castration-resistant prostate cancer.

Single nucleotide polymorphism (SNP) genotyping could be used to predict radiation dermatitis in patients with breast cancer.

Increasing the number of intravenous port nurse champions across a health care system helps to keep oncology nurses with their patients and reduce care delays.

The death doula is a unique role that can help oncology care teams improve the quality of end-of-life care delivered to patients.

The addition of apalutamide to androgen deprivation therapy does not lead to a significant patient-reported side effect burden nor a reduction in health-related quality of life in patients with metastatic castration-sensitive prostate cancer.

Patients with cancer were reported to have mixed expectations with immunotherapy as part of their oncology treatment.

The addition of ublituximab and umbralisib (Ukoniq; U2) to ibrutinib (Imbruvica) demonstrated a 77% undetectable minimal residual disease (uMRD) rate in patients with chronic lymphocytic leukemia.
Laura Zitella, MS, RN, ACNP-BC, AOCN, discusses third-line treatment options for patients with diffuse large b-cell lymphoma.

Point-of-use shower filtration may be an effective strategy in reducing waterborne pathogens and protecting patients who underwent stem cell transplant from infection.
A patient-friendly stoplight tool with 3 different colored zones helped patients undergoing chemotherapy manage diarrhea and reduce hospital and emergency department visits.

Patients who receive medical cannabis in addition to standard opioids may require less overall opioid treatment to manage their pain.
Specialty nurse practitioners can help tailor pain management programs for patients with sickle cell disease and decrease hospital stay times.

Independent verification of documentation is paramount to patient safety.

The framework for establishing equity, diversity, and inclusion throughout oncology nursing already exists within the standard for health and safety, explains Aliènne Salleroli, MS, BSN, RN, OCN.

An implementation of nursing practice changes helped improve the fall rates among patients being treated by the surgical oncology team.