
A multidisciplinary care team is needed when treating patients who are given a combination of chemotherapy and immunotherapy.

A multidisciplinary care team is needed when treating patients who are given a combination of chemotherapy and immunotherapy.

PD-L1 status may not be the best predictor when it comes to determining who will respond to checkpoint blockade.

Combining two checkpoint blockades can be very efficacious in treating metastatic melanoma, but the benefits come with increased risk of adverse events, too.
Managing immune-related adverse events is different from managing the effects of chemotherapy.

An expert goes over the common – and not-so-common – immune-related adverse events.

Researchers are working on a way to spark the immune response against glioblastoma, making the nurses’ role in treatment even more important.

The FDA granted a priority review to the supplemental biologics license application for pembrolizumab (Keytruda) for the first-line treatment of patients with recurrent or metastatic head and neck squamous cell carcinoma (HNSCC).
Immunotherapy agents may soon combine with VEGF TKIs to redefine the frontline standard for treatment of metastatic renal cell carcinoma (mRCC).

Pembrolizumab (Keytruda) was found to reduce the risk of death by 31% in patients with PD-L1–positive (combined positive score [CPS] ≥10) advanced or metastatic esophageal or esophageal junction carcinoma who progressed on standard therapy, according to phase III findings of the KEYNOTE-181 trial.

Two-thirds of patients with untreated metastatic HER2-positive esophagogastric adenocarcinoma remained free of disease progression at 6 months with a combination of pembrolizumab (Keytruda), trastuzumab (Herceptin), and chemotherapy, a small clinical trial showed.

Howard Cohen, RPh, MS, FASHP, director of oncology pharmacy services, Smilow Cancer Center, Yale New Haven Health, discusses the challenges of cancer treatment from a pharmacy perspective.
Improvements observed in progression-free survival and overall survival with the addition of first-line atezolizumab (Tecentriq) to nab-paclitaxel (Abraxane) in patients with metastatic triple-negative breast cancer (TNBC) or inoperable locally advanced TNBC are exclusive to those patients with PD-L1 expression ≥1% in immune cells, according to a biomarker subgroup analysis of the phase III IMpassion130 study.1

Oncology nurses must not only be aware of the adverse events (AEs) of immunotherapy, but they must also educate their patients—and their other healthcare providers—to recognize them as well, according to Massey Nematollahi, MScN, RN, CNS, OCN, CON.

The FDA has approved the combination of atezolizumab (Tecentriq), bevacizumab (Avastin), carboplatin, and paclitaxel (ABCP) for the frontline treatment of metastatic nonsquamous non-small cell lung cancer (NSCLC). This indication excludes patients with EGFR/ALK aberrations.

ACCC worked closely with a team of multispecialty thought leaders via the IO Institute Working Groups to develop forward-thinking resources at the intersection of clinical science, care delivery, business, operations, and policy to support all facets of immunotherapy integration.

Kathy Oubre, MS, Chief Operating Officer, Pontchartrain Cancer Center in Covington, Louisiana, shares some barriers to adherence to oral oncolytics that patients may face.

The PD-1 inhibitor pembrolizumab (Keytruda) has shown an overall survival advantage across 3 phase III clinical trials studying its use in patients with metastatic non–small cell lung cancer (NSCLC). These positive results led to a frontline indication as a single agent and in combination with chemotherapy for both patients with squamous and nonsquamous NSCLC.

Not enough is known about immunotherapy-related adverse events, so it is important to report unusual or previously unreported ones to the FDA.
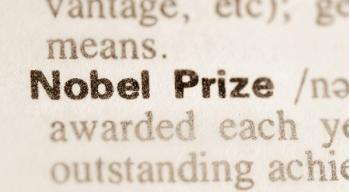
Immunotherapy pioneers James P. Allison, PhD, and Tasuku Honjo, MD, PhD, have won the 2018 Nobel Prize in Physiology or Medicine for their research that eventually led to the use of immune checkpoint inhibitors to treat cancer.

The FDA has granted a priority review to the immunostimulatory monoclonal antibody elotuzumab (Empliciti) for use in combination with pomalidomide (Pomalyst) and low-dose dexamethasone (EPd) to treat patients with relapsed/refractory multiple myeloma (MM) who have received 2 or more prior therapies, including lenalidomide (Revlimid) and a proteasome inhibitor.

A year after the first CAR T-cell therapy was approved to treat pediatric patients with relapsed and/or refractory CD19-positive acute lymphoblastic leukemia (ALL), researchers have issued guidelines to help healthcare professionals recognize and treat the associated adverse events (AEs) from this treatment.

CE lesson worth 1 contact hour that is intended to advanced practice nurses, registered nurses, and other healthcare professionals who care for patients with cancer.

The FDA granted an accelerated approval to the immunotherapy combination of nivolumab (Opdivo) and ipilimumab (Yervoy) for use in adult and pediatric patients 12 years and older with microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) metastatic colorectal cancer (mCRC) following progression on a fluoropyrimidine, oxaliplatin, and irinotecan.

These are the most popular stories posted on Oncology Nursing News in the month of June.
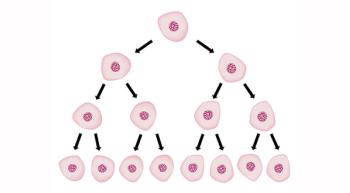
An off-the-shelf, dual-targeted chimeric antigen receptor (CAR) T-cell approach yielded positive results in preclinical specificity, functionality, and efficacy studies.
A promising CD19-directed chimeric antigen (CAR) T-cell therapy, Lisocabtagene maraleucel (JCAR017; liso-cel), may result in durable remissions among patients with high-risk diffuse large B-cell lymphoma (DLBCL), the most common type of non-Hodgkin lymphoma.

Patients with relapsed/refractory heavily pretreated multiple myeloma could live for an extra progression-free year with the use of the anti-BCMA CAR T-cell therapy bb2121.

Immuno-Oncology (IO) and novel agents targeting the microenvironment were the focus of the 2018 annual meeting of the American Society of Clinical Oncology (ASCO).

Cancer immunotherapies are a promising development, but taking care of patients who are using these drugs can be a challenge for oncology nurses.

CE lesson worth 1 contact hour that is intended to advanced practice nurses, registered nurses, and other healthcare professionals who care for patients with cancer.