Breast Cancer
Latest News
Latest Videos

More News

ASCO recently issued practice guidelines for pathologic diagnosis of breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL) to help healthcare practitioners better this rare disease.

Here are the top 5 Oncology Nursing News® stories for February 2020.

The FDA has approved a supplemental new drug application (sNDA) for neratinib (Nerlynx) in combination with capecitabine (Xeloda) for the treatment of adult patients with advanced or metastatic HER2-positive breast cancer who have received ≥2 prior anti–HER2-based regimens in the metastatic setting.

The FDA has accepted a Biologics License Application (BLA) for a fixed-dose combination (FDC) of pertuzumab (Perjeta) and trastuzumab (Herceptin) with hyaluronidase, administered by subcutaneous (SC) injection in combination with intravenous (IV) chemotherapy, for the treatment of eligible patients with HER2-positive breast cancer.

The fields of early-stage hormone receptor (HR)–positive and metastatic HER2-positive breast cancer have made great strides in recent years, said Neelima Denduluri, MD, and such progress could be attributed to the emergence of tailored treatment strategies and the use of HER2-directed agents, respectively.


The frontline combination of pembrolizumab (Keytruda) and chemotherapy significantly improved progression-free survival (PFS) compared with chemotherapy alone in patients with metastatic triple-negative breast cancer (TNBC) whose tumors expressed PD-L1 (combined positive score [CPS] ≥10), meeting one of the dual primary endpoints of the phase III KEYNOTE-355 trial.

Nearly 1 year following the first checkpoint inhibitor approval in advanced triple-negative breast cancer, additional immunotherapeutic agents are poised to enter the field, according to Rita Nanda, MD.

Despite the emergence of PARP inhibitors, antibody-drug conjugates (ADCs), and immunotherapy in the treatment of patients with triple-negative breast cancer (TNBC), more work is needed to propel further progress, according to Kevin Kalinsky, MD, MS.
Combining ovarian suppression and an aromatase inhibitor is an efficacious treatment method for premenopausal women with breast cancer. However, the regimen (which is given long-term) can cause some major adverse events, explained Dawn L. Hershman, MD, MS, professor of medicine and epidemiology at the Columbia University Irving Medical Center.
The role of radiation therapy, specifically with elective nodal irradiation (ENI), has evolved over the past several years, said He James Zhu, MD, PhD, adding that the technique should be performed in patients with breast cancer on an individualized basis.

Research presented at the 2019 San Antonio Breast Cancer Symposium (SABCS) had a significant effect on the standard of care for patients with HER2-positive metastatic breast cancer, explained Erika P. Hamilton, MD.

Frequent communication between patients and providers is key in getting ahead of adverse events that can occur during breast cancer treatment, explained Madeline Kuiper, MSN, RN, OCN, an oncology nurse practitioner at UCLA.
While the regimen was overall well tolerated, there are some adverse events for nurses to look out for.
The FDA has accepted a biologics license application (BLA) to review eflapegrastim (Rolontis) for the management of chemotherapy-induced neutropenia, according to Spectrum Pharmaceuticals, the developer of the novel long-acting granulocyte-colony stimulating factor (G-CSF).

The FDA has accepted a biologics license application (BLA) for sacituzumab govitecan as a treatment for patients with metastatic triple-negative breast cancer (TNBC) who have received at least 2 prior therapies for metastatic disease, according to a statement from the company developing the antibody-drug conjugate (ADC), Immunomedics.

The FDA has approved the use of Trastuzumab Deruxtecan for the treatment of patients with HER2+ Breast Cancer, based on recent findings.

The FDA has granted tucatinib a breakthrough therapy designation for use in combination with trastuzumab (Herceptin) and capecitabine (Xeloda) for the treatment of patients with unresectable locally advanced or metastatic HER2-positive breast cancer, including patients with brain metastases, who had prior trastuzumab, pertuzumab (Perjeta), and ado-trastuzumab emtansine (T-DM1; Kadcyla).

It is important that nurses talk with their patients about what kind of adverse events to expect while being treated for HER2-positive breast cancer.

Residual cancer burden (RCB) after neoadjuvant chemotherapy has been shown to be an accurate long-term predictor of disease recurrence and survival across all breast cancer subtypes, according to data from a large meta-analysis presented at the 2019 San Antonio Breast Cancer Symposium.
A durvalumab (Imfinzi)-based neoadjuvant regimen induced a pathologic complete response (pCR) rate of 44% in patients with triple-negative breast cancer (TNBC), according to results of a phase I/II study presented in a poster at the 2019 San Antonio Breast Cancer Symposium.

Real-world clinical practice results for frontline palbociclib (Ibrance) indicate that the positive progression-free survival (PFS) data previously reported with the CDK4/6 inhibitor in the pivotal PALOMA-2 trial would likely translate to an overall survival (OS) benefit in patients with HR-positive/HER2-negative metastatic breast cancer.
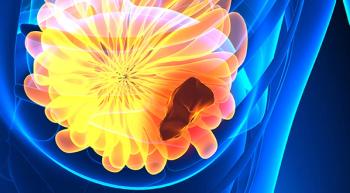
Trastuzumab deruxtecan had an ORR rate of nearly 61% for patients with advanced HER2-positive breast cancer.

The FDA has approved 2 abbreviated new drug applications (ANDAs) for everolimus (Afinitor) tablets for the treatment of patients numerous malignancies.