
Criteria for progression-free and overall survival endpoints in patients with endometrial cancer with mismatch repair proficient disease were not met.

Criteria for progression-free and overall survival endpoints in patients with endometrial cancer with mismatch repair proficient disease were not met.

Trial data support potential treatment options with durvalumab-based regimens for advanced or recurrent endometrial cancer.
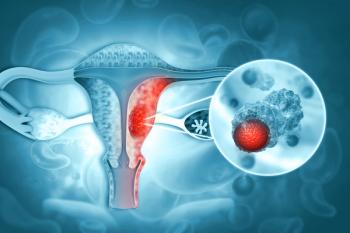
Patients across endometrial cancer subgroups derived a favorable survival benefit with pembrolizumab plus chemotherapy in the KEYNOTE-868 trial.

Patients with microsatellite instability high primary advanced or recurrent endometrial cancer derived a significant survival benefit when treated with dostarlimab plus chemotherapy.

Patients with platinum-resistant or -refractory epithelial ovarian cancer treated with olaparib plus cediranib did not experience improvements in PFS and OS compared with chemotherapy.

Further evidence strengthens the support of mirvetuximab soravtansine as a new standard of care for folate receptor-alpha—positive ovarian cancer resistant to platinum chemotherapy.

Although frontline treatment with lenvatinib plus pembrolizumab improved ORR and PFS, it did not improve OS when compared with placebo in patients with head and neck squamous cell carcinoma.

Patients with metastatic urothelial cancer treated with frontline maintenance therapy with avelumab following platinum-based chemotherapy in the real-world setting had similar outcomes as observed in the JAVELIN Bladder 100 trial.

Patients with hematologic malignancies who received Orca-T improved survival rates compared with PTCy in those receiving myeloablative conditioning, according to findings from a retrospective analysis.

Immune engager therapies, according to a retrospective study of real-world patients, had the best rates of responses and progression-free survival in patients with multiple myeloma whose disease relapsed after treatment with idecabtagene vicleucel.

Patients with relapsed/refractory chronic lymphocytic leukemia or small lymphocytic lymphoma treated with lisocabtagene maraleucel experienced durable responses.

The antifungal prophylaxis azoles did not impact the safety and efficacy of ruxolitinib in patients with graft-vs-host disease.

Patients with GVHD treated with ruxolitinib plus belumosudil experienced an overall response rate of 55%, which may suggest an interaction between inflammatory pathways.

Compared with placebo, ruxolitinib cream significantly improved body surface area in patients with cutaneous graft-vs-host disease in a phase 2 trial.
It may be feasible to use brexucabtagene autoleucel for the treatment of patients with relapsed/refractory B-cell acute lymphoblastic leukemia with central nervous system involvement.
Liso-cel may be an effective treatment option for relapsed/refractory mantle cell lymphoma, including those with high-risk features who have limited treatment options.

Patients with BRCA-, ATM- and CDK12-mutated mCRPC treated with frontline olaparib plus abiraterone acetate experienced delays in disease progression and improved outcomes.

Subsequent therapies in patients with metastatic hormone-sensitive prostate cancer who were censored from primary overall survival follow-up from the ARASENS trial, according to a post hoc sensitivity analysis, confirmed the overall survival benefit derived from darolutamide plus androgen deprivation therapy and docetaxel.

Favorable ECOG performance status and less advanced disease may predict which patients with metastatic colorectal cancer might have long-term remission when treated with regorafenib.

After radical prostatectomy, patients with prostate cancer treated with abiraterone acetate plus prednisone and apalutamide had improved outcomes without a significant impact on their health-related quality of life.
First-line treatment with nivolumab plus ipilimumab for patients with microsatellite instability–high or mismatch repair deficient metastatic colorectal cancer can be considered a standard-of-care option based on results from the phase 3 CheckMate-8HW trial.

Treatment with belzutifan for advanced/metastatic clear cell renal cell carcinoma delayed worsening symptoms and improved quality of life.
Researchers did not observe any grade 3 or 4 adverse events with darolutamide with androgen deprivation therapy for 6 months followed by radical prostatectomy in patients with locally advanced prostate cancer.

All patients enrolled in the EV-302 trial with previously untreated, locally advanced, or metastatic urothelial carcinoma obtained a survival benefit with enfortumab vedotin-ejfv plus pembrolizumab.

Cabozantinib plus atezolizumab may be a new treatment option for patients with metastatic castration-resistant prostate cancer whose disease progressed on novel hormonal therapy.

Patients with cisplatin-ineligible urothelial carcinoma treated with frontline pembrolizumab plus cabozantinib obtained responses with a manageable toxicity profile.
Patients with high-risk prostate cancer treated with a higher dose of radiation therapy and long-term androgen deprivation therapy improved progression-free, cancer-specific, and overall survival compared with the standard dose of radiation.
Frontline olaparib plus abiraterone/prednisone improved progression-free survival and responses in patients with metastatic castration-resistant prostate cancer compared with each of the components of the therapy alone.

Patients with metastatic castration-resistant prostate cancer who were previously treated with external beam radiation therapy before radium-223 did not experience an increase in hematological toxicity compared with the overall population.

Despite germline and somatic testing being the standard of care for patients with metastatic castration-resistant prostate cancer, rates of its real-world use shows that it may be underutilized, which may negatively impact therapeutic offerings.